Goals
Under California’s “Master Plan for Higher Education,” the University of California is delegated the primary responsibility in public higher education for doctoral education. For the health professions, this means that UC is the only California public institution chartered to grant the following professional degrees: D.D.S. (Doctor of Dental Science), M.D. (Doctor of Medicine), O.D. (Doctor of Optometry), Pharm.D. (Doctor of Pharmacy) and D.V.M. (Doctor of Veterinary Medicine). Along with other private educational institutions, UC also provides doctoral education leading to Ph.D. degrees in Nursing and Public Health, as well as the Dr.P.H. (Doctor of Public Health) degree.
UC health sciences programs are national and international leaders in teaching, research and clinical care. In support of these programs, UC provides leadership and strategic direction to advance the missions of the University’s 17 health professional schools and 12 hospitals, referred to collectively as UC Health1
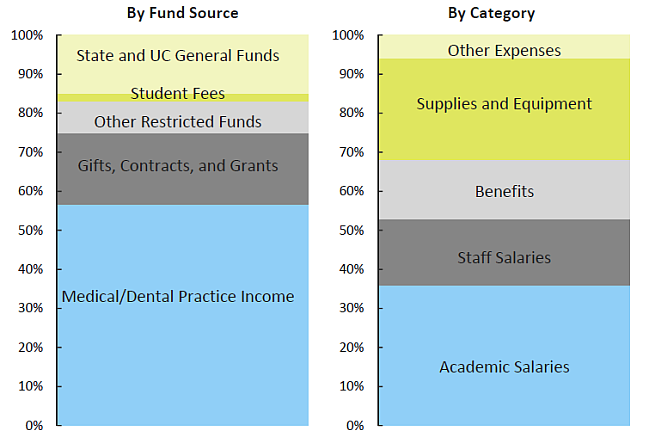
UC’s mission of instruction, research and public service is carried out across the entire system, but a great portion of the service activity, measured in terms of operating expenditures, occurs under the auspices of UC Health. In 2013–14, operating expenditures for UC Health rose to about $12 billion, almost 45 percent of the University’s total operating expenditures. Of this amount, $2.4 billion represented instructional activities, $1.8 billion was spent on research, and $7.3 billion was expended by the medical centers in the delivery of health care services.
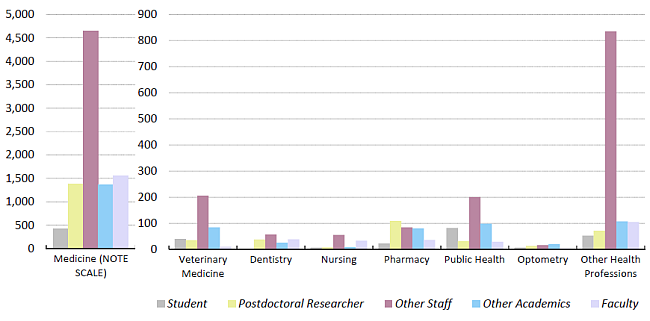
In fall 2014, about 35 percent of all UC faculty worked in health science disciplines. These faculty made up about one-sixth of all ladder-rank faculty and more than one-half of all other faculty across the UC system. Ladder-rank faculty have duties primarily focused on teaching and research. Other faculty are primarily clinical faculty; other academics are primarily researchers.
In fall 2014, 43 percent of postdoctoral fellows were in health science disciplines.2
Educating health care professionals
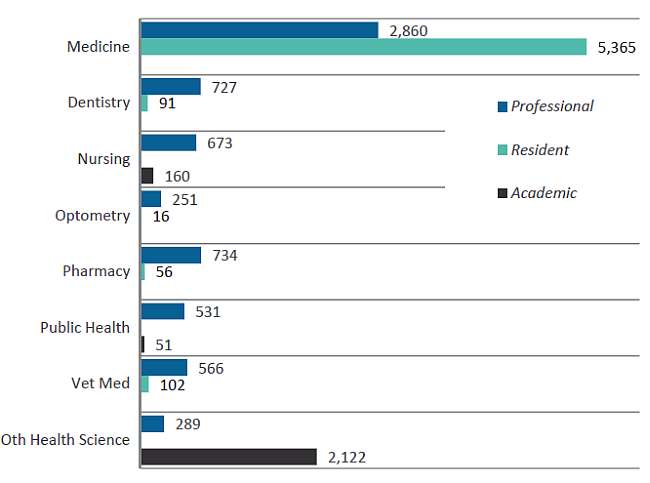
The University of California operates the largest health sciences instructional program in the nation, enrolling more than 14,000 students annually. The systemwide instructional program includes six schools of medicine and three smaller medical education programs (located in Berkeley, in Fresno and at the Charles R. Drew University of Medicine and Science in Los Angeles); three schools of nursing (and one program in nursing science at Irvine); two schools each of dentistry, pharmacy and public health; and one school each of optometry and veterinary medicine. The long-standing medical education program that operated jointly between UC Riverside and UCLA for more than 30 years transitioned in 2013 to an independent UC medical school.
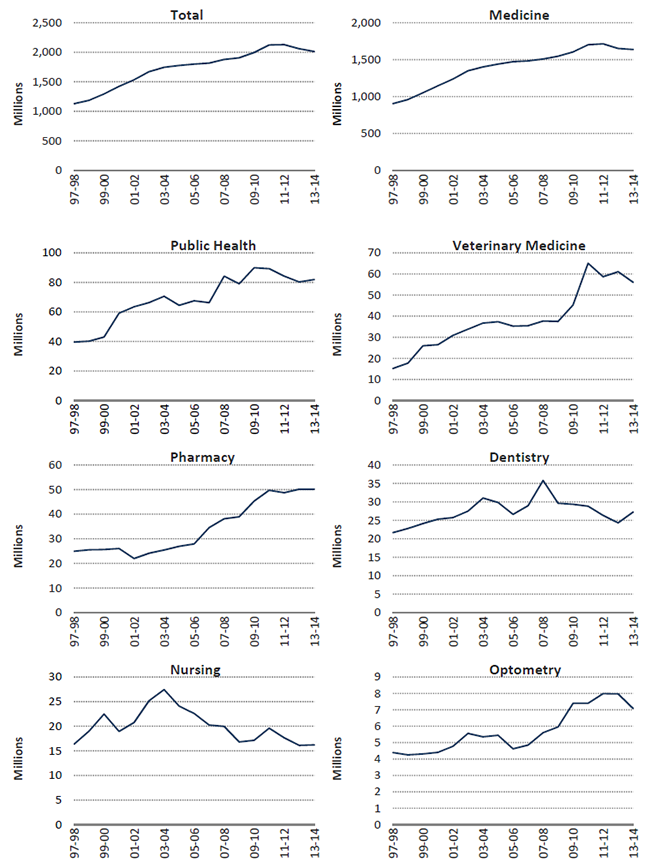
A focus on medical research
Health science research expenditures represent the single largest disciplinary focus of UC’s research enterprise. Half of UC’s total research expenditures were for medical research, including related fields such as public health and veterinary medicine. More than half of the funding for this medical research was provided by federal agency awards to UC.
Clinical trial research is an increasingly important component of UC’s medical research enterprise. During 2013–14, there were more than 2,800 clinical trials underway systemwide, and of the $2.3 billion UC received that year in medical research awards, about 17 percent of the total was targeted for clinical trials. More than 80 percent of these clinical trial projects were sponsored by businesses.
These clinical trials occupy a unique position in UC’s research enterprise. They represent the final stage in the journey from a scientific discovery or innovation to an effective therapy or treatment that could significantly enhance global health.
Keeping California healthy
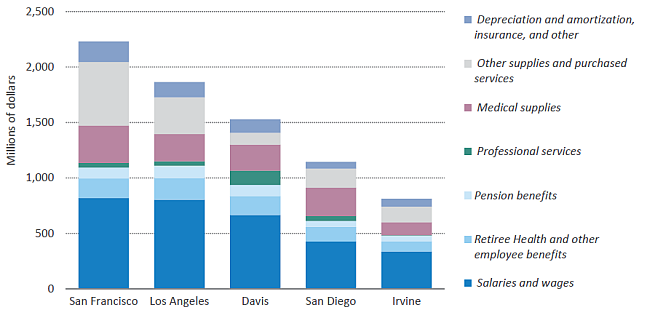
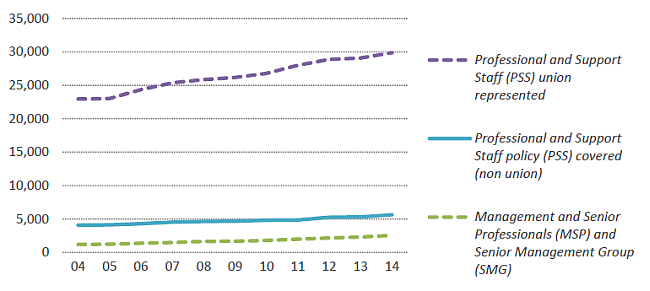
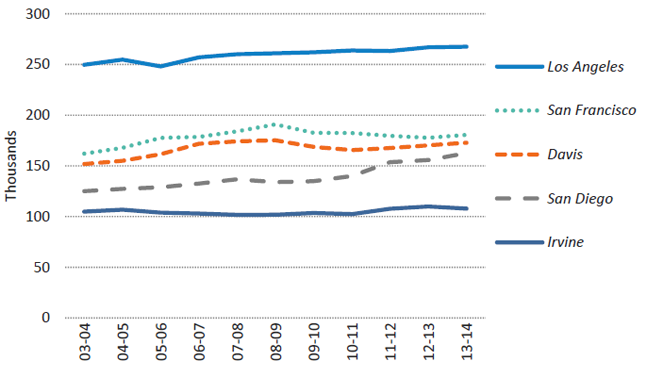
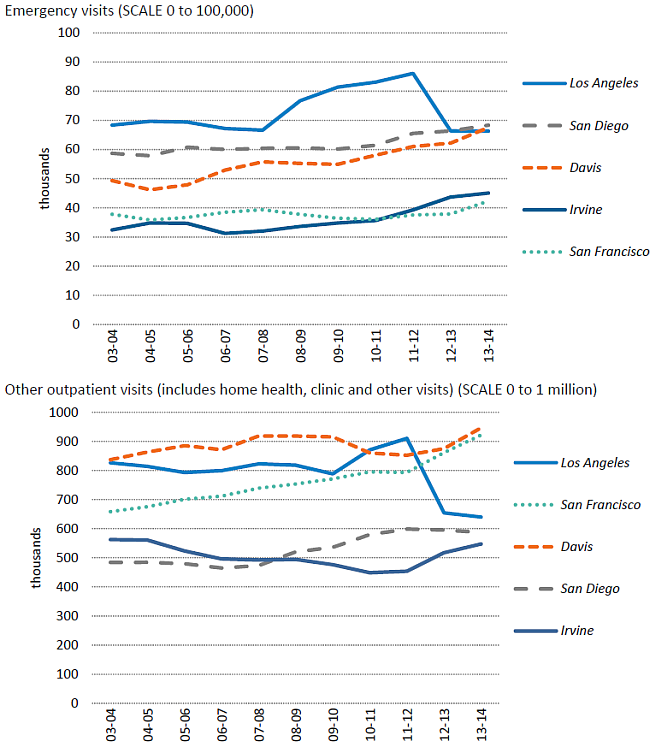
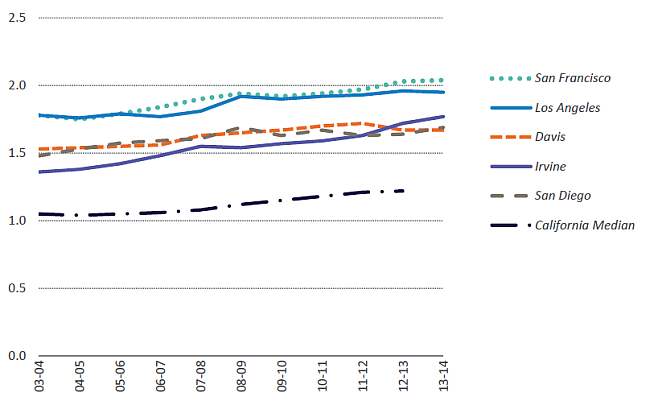
The University of California’s five academic medical centers (Davis, Irvine, Los Angeles, San Diego and San Francisco) provide a vast resource for the clinical training programs of UC health professional schools. These centers prepare future generations of health professionals; they catalyze major advances in biomedical and clinical research; and they serve as California’s fourth-largest health care delivery system, with about 42,000 employees, including approximately 12,000 nurses. UC operates or staffs five major trauma centers, providing half of all transplants and one-fourth of extensive burn care in the state. UC hospitals are also designated as Ebola treatment centers for the state. UC medical centers manage more than 159,000 inpatient admissions, 334,000 emergency room visits and 4.2 million outpatient visits each year. Nearly 60 percent of UC patients are covered by Medicare or Medi-Cal, or lack health insurance. In support of its teaching, research and public service missions, UC health programs also maintain active relationships with more than 100 affiliated Veterans Affairs, county and community-based health facilities located throughout California.
In view of the size and contributions of health-related programs across the UC system, select performance indicators related to students, faculty and research are included both in this chapter and in the respective sections of this report that are devoted to those subject areas. For example, indicators related to students enrolled in UC professional degree programs are also included in Chapter 4 (Graduate Academic and Graduate Professional Degree Students). Chapter 5 (Faculty and Other Academic Employees) includes indicators related to UC faculty appointments, headcounts and conference of doctoral degrees. Information regarding diversity is found in Chapter 7. Research workforce indicators for medicine and health sciences, as well as indicators for general funding and expenditures, are included in Chapter 9 (Research — Increasing Public Knowledge).
In addition, this chapter includes information and performance indicators for various aspects of the University’s health sciences system, including information regarding health professional degree students, health sciences instruction and research expenditures, and the health sciences academic workforce. This section also includes a number of indicators and metrics related to the University’s health care delivery system.
Looking forward
California’s population is growing, aging and increasing in diversity. Already the most populous state in the nation, California’s population is projected by the Department of Finance to grow 39 percent from 2012 to 2060. Statewide shortages and maldistribution of health providers already exist in many health professions. These challenges will grow as health care reforms drive increasing demand for quality and accountability in the delivery of health services. At a time of unprecedented budgetary challenges, the financial success of UC medical centers has been an important resource for helping to back-fill diminishing state support for UC schools of medicine. However, the changing environment for health care signals changes that threaten this financial success and the ability of the medical centers to help support the academic mission of UC medical schools. Among these financial challenges are 1) reductions in federal and state spending for programs such as Medicare, Medi-Cal and the National Institutes of Health; and 2) challenges associated with the implementation of health care reform.
Notwithstanding these challenges and the uncertainties related to health reform, UC Health is working to support new initiatives and developments to help meet current and future health care needs. Within the health professions, these include the opening of the Betty Irene Moore School of Nursing at UC Davis; the creation of new programs, at each UC medical school, in medical education focusing specifically on the needs of medically underserved communities; and the opening of a new medical school at UC Riverside, concentrating on the needs of California’s Inland Empire, making UCR the first new allopathic (M.D.-granting) medical school to open in California in more than 40 years.
To recognize and accelerate implementation of innovative practices in clinical care, UC Health launched the UC Center for Health Quality and Innovation in 2010. The center promotes innovations in clinical care that improve patient outcomes and quality of care within the UC system and beyond. These and other activities are among the many initiatives now underway at UC to help improve quality, access and value in the delivery of health services.
Leveraging Scale for Value
The Leveraging Scale for Value initiative is the systemwide approach to cost reduction in the UC Health clinical enterprise. The activity focuses on four areas — supply chain, revenue cycle, clinical laboratories and information technology — with a goal of achieving a $150 million to $200 million reduction in expenses each year for five years. UC Health is on target for a $50 million decrease in supply chain expenses for fiscal year 2015. The revenue cycle activities are on target for a yearly recurring benefit of $108 million to $143 million.
1 Data in this chapter exclude UCSF Benioff Children’s Hospital Oakland except where noted.
2 Statistics are by headcount rather than FTE. Headcount numbers tend to be larger than FTE, especially in the health sciences, because non-ladder-rank health science faculty, such as clinical faculty, are more likely to have joint or partial appointments.
FOR MORE INFORMATION
The UC Health website provides an in-depth description of UC Health facilities and activities.