History
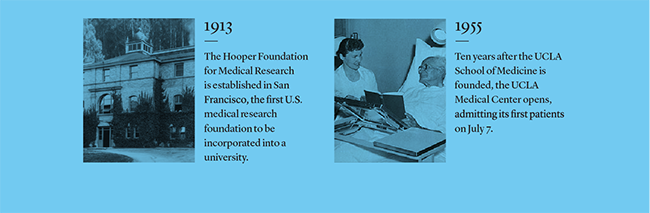
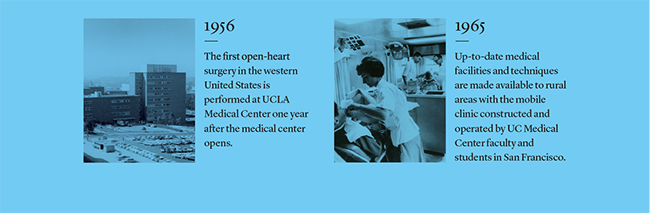
When state assemblyman John Dwinelle prepared the charter for the University of California in 1868, he had the foresight to call for the formation of a college of medicine “and other like professional colleges.” In 1873 the Toland Medical College of San Francisco joined the University and became the University’s first professional school. In 1881, UC established the first dental school west of the Mississippi River. UC continued its expansion of medical and health professional schools through the end of the nineteenth century, all of the twentieth century and into the twenty-first century with the recent addition of a School of Nursing at Irvine in 2017.
The scope of UC Health
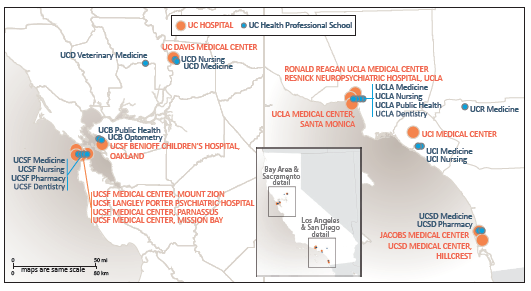
Today, the University’s 18 health sciences schools and five academic medical centers—organized as UC Health—are international leaders in the education of health professionals, in research that develops new cures and treatments, and in public service that provides health care for all Californians regardless of ability to pay.
In June 2017, the first students graduated from UC Riverside Medical School, the sixth medical school in the system.
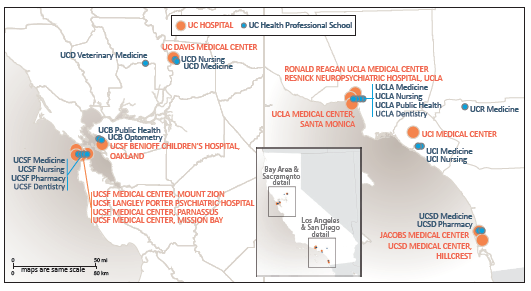
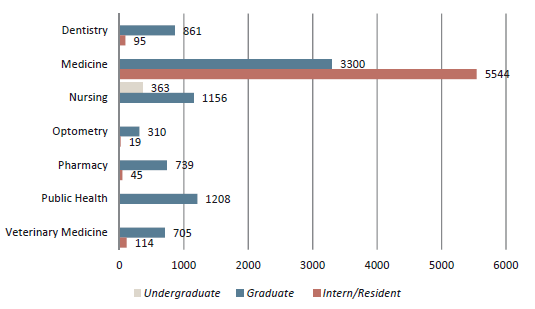
UC’s health sciences schools are:
- Dentistry (UCSF, UCLA)
- Medicine (UCD, UCSF, UCLA, UCR, UCI, UCSD)
- Nursing (UCD, UCSF, UCLA, UCI)
- Optometry (UCB)
- Pharmacy (UCSF, UCSD)
- Public Health (UCB, UCLA)
- Veterinary Medicine (UCD)
UC’s health science schools are among the best in the nation, according to U.S. News & World Report 2019 rankings.
US News & World Report’s “Best of” Rankings as of 2019:
| |
UCSF |
UCLA |
UCSD |
UCD |
UCI |
UCB |
UCR |
| Best Medical Schools – Research |
5 |
8 |
22 |
39 |
46 |
|
93 |
| Best Medical Schools – Primary Care |
2 |
4 |
17 |
10 |
77 |
|
|
| Best Nursing Schools – Masters |
11 |
20 |
|
46 |
66 |
|
|
| Best Graduate Public Health |
|
10 |
|
|
|
9 |
|
| Best Pharmacy Schools |
3 |
|
25 |
|
|
|
|
| Best Veterinary Medicine Schools |
|
|
|
1 |
|
|
|
Note: USN&WR does not rank dental or optometry programs.
All across the state, each of UC Health’s academic medical centers has earned a place among U.S. News & World Report’s “Best Hospital” rankings, as shown in the table below:
| Best Hospitals - Nationally |
Best Hospitals - California |
| #5 UCSF |
#1 UCSF |
| #7 UCLA |
#2 UCLA |
| |
#5 UCD |
| |
#7 UCSD |
| |
#11 UCI |
Residency programs — increasingly funded without federal support
Graduate Medical Education (residency) programs provide in-depth training in specialties of medicine after graduation from medical school. All of UC’s academic medical centers provide residency programs and fund an increasing number of them without traditional federal support. In the 1960s, Medicare began paying for a substantial portion of the cost of residency programs. In 1997, it limited the number of residencies that would be funded, and the ‘cap’ has not been revised upward despite a 30 percent increase nationally in the number of medical students and an aging population that needs more practitioners. As a result, UC medical centers began absorbing costs for residency training slots. In FY 2017–18, UC Health trained 5,540 residents through UC-sponsored and long-standing UC-affiliated family medicine programs–or approximately half of California’s total. This includes 594 positions for which UC received no federal General Medical Education support and covered roughly $59 million in unreimbursed costs.
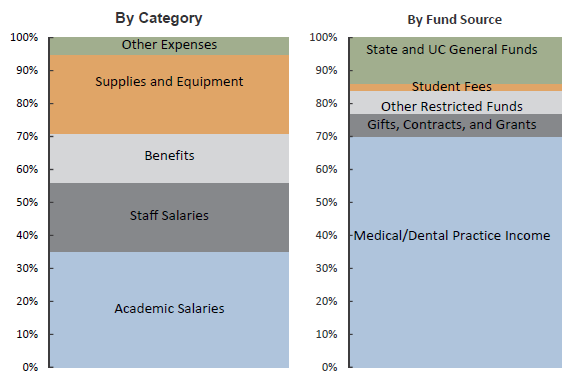
Medical Centers — clinical operations are self-supporting
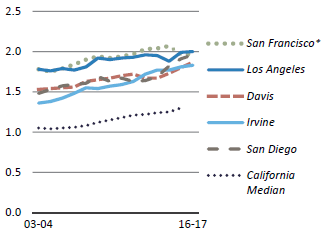
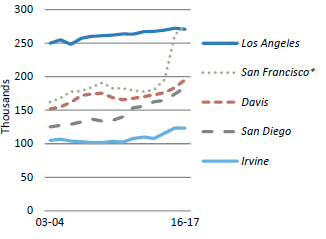
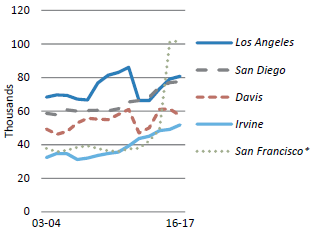
UC Health’s medical centers receive no state general funds. Clinical operations at the five academic medical centers—UC Davis Health, UCSF Health, UC Irvine Health, UCLA Health and UC San Diego Health—are supported by insurance reimbursements from governmental and commercial payers. Additionally, the medical centers provide financial support to UC Health Schools of Medicine to fund operating activities, clinical research, faculty practice plans and other programs. In FY 2017, the support was $457 million.
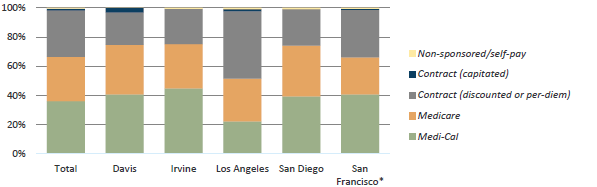
Inpatient days by coverage type, FY 16-17
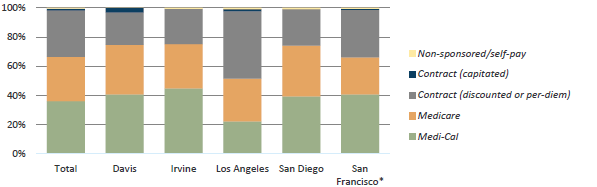
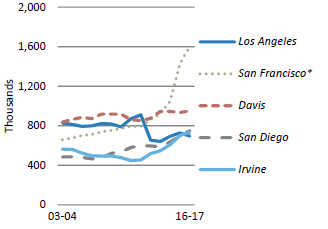
*San Francisco data includes UCSF Medical Center, Children’s Hospital & Research Center Oakland (CHRCO), and the activities of UCSF Medical Group.
Source: UC Health
As shown above, coverage types for inpatient days across the system are 36 percent Medi-Cal, 30 percent Medicare and 32 percent commercial contracts, with the remainder uninsured or self-pay. Medi-Cal reimbursement covers an estimated 50 to 60 percent of the cost of care per patient, while Medicare covers 90 percent. Higher commercial insurance reimbursements help fill the funding gap.
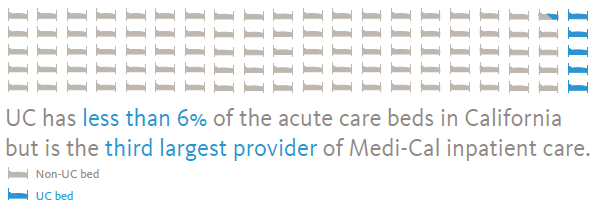
Medi-Cal – the commitment to all Californians
UC Health hospitals provide primary care to managed Medi-Cal beneficiaries and provide for specialty services, reflecting the system’s traditional strength in tertiary and quaternary care. Almost one-third of Californians are now covered by Medi-Cal. UC Health values the significant role Medi-Cal plays in preserving and improving the health of the state. UC Health hospitals comprise less than six percent of the licensed general acute care staffed hospital beds in California, yet are the third largest provider of inpatient days for Medi-Cal beneficiaries.
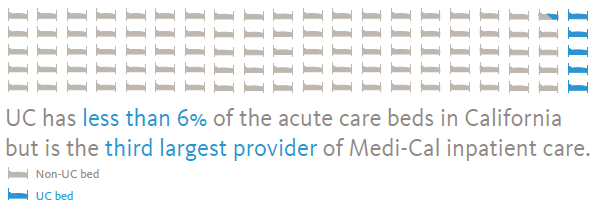
Source: American Hospital Directory cites 74,925 non-federal, short-term, acute care staffed hospital beds in CA.
For outpatient care, UC Health’s clinics are the fourth-largest provider of care in the state for Medi-Cal beneficiaries, with more than 750,000 visits per year.
The expansion of Medi-Cal in 2014 through the Patient Protection and Affordable Care Act (ACA) increased enrollment by nearly 60 percent. Expansion costs initially were borne almost entirely by the federal government, but by 2020, ten percent will be borne by the state. As financial responsibilities shift to California, this will present a financial challenge to the state and all safety net hospitals, including UC Health.
In FY 2017, UC Health provided more than $250 million in charity care and an additional estimated $914 million in uncompensated care for patients in publicly sponsored programs.
Growing affiliations — extending clinical care beyond UC’s facilities
UC Health campuses are expanding their delivery networks through clinical affiliations with hospital systems or Federally Qualified Health Centers (FQHC). These efforts create opportunities to enhance clinical quality, provide direct patient care and advance the system’s educational missions outside the walls of UC-owned facilities. UC residents at these facilities provide care to Medi-Cal, Medicare and commercially insured patients. Agreements for clinical coordination may include primary care and obstetrical services or specialized services such as oncology care, neurosurgery and liver transplantation.
The future — strategic plan and system integration
Health care is rapidly changing. To meet this challenge, the campus and system leadership of UC Health crafted a multi-year strategic plan (2017–2022) to advance the tripartite missions of public service clinical care, research and education. Integral to the plan is a recognition that the future requires collaboration across locations.
The world-class expertise at each campus—when connected to like-minded colleagues at other sites—holds great promise for Californians and people around the world. Some examples include:
More than $700 million in savings & counting—Leveraging Scale for Value
UC Health has a fiduciary responsibility to the state and system to manage scarce resources wisely. One of the earliest systemwide collaborations is the Leveraging Scale for Value initiative (LSfV), which works on supply chain, revenue cycle and information technology improvements. This project saved $182.5 million in FY 2015, $261 million in FY 2016, and $286 million in FY 2017 for cumulative savings of more than $729. The LSfV strategy also taps into site-specific expertise for the benefit of the system. For example, the information technology team at UCSD extended the same instance of EPIC electronic medical records (EMR) at UC Irvine Health.
Clinical & Research Collaboration—power of scale
While cost reduction is important in any organization, UC Health views its principal objective as leveraging the collective scientific acumen and learnings across the UC system to develop the clinical care standard for the future.
Below are a few examples.
UC BRAID—all UC clinical trials in one place
The University of California Biomedical Research Acceleration, Integration and Development program (UC BRAID) is recognized by the National Institutes for Health (NIH) as a cutting-edge consortium for conducting clinical and translational research. Its accomplishments include creating a master database of all Institutional Review Board (IRB)-approved clinical trials in the consortium, creating an easier way for patients and physicians to find trials regardless of location. UC BRAID also built a research exchange, UC ReX, to simplify access to more than 15 million de-identified patient records across the system, and streamlined approvals of multi-site biomedical research programs.
Cancer Center Consortium—five NCI-designated centers with a shared goal
In fall 2017, the cancer centers within UC Health joined forces in a consortium to accelerate research and improve patient outcomes. There are approximately 1,500 cancer centers in the U.S., but only 49 have achieved the highest designation—Comprehensive Cancer Center—meaning they demonstrate scientific leadership, provide early phase innovative clinical trials, operate substantial research programs and are a source of expertise. UC Health is the only health system in the nation with five NCI-designated comprehensive cancer centers.
Each year, more than 170,000 Californians are diagnosed with cancer. Nearly 60,000 annually die from it. UC’s Cancer Consortium is taking a leadership role by providing clinical trials using the latest experimental drugs, matching drugs to cancer subtypes and rare tumors, developing precision medicine technology, harnessing big data and working to reduce socioeconomic disparities in access to care.
Cardiothoracic Surgery—improving heart, lung and esophagus care
More than eight million Californians have some form of heart disease. The fourth leading cause of death in the state is lung disease. These and other medical conditions in the chest are tackled by cardiothoracic surgeons.
UC Health’s cardiothoracic surgeons began a collaboration in 2012 to improve outcomes, reduce practice and outcome variability across the five medical centers, and reduce overall cost and cost variability at each center. Through performance dashboards, national benchmarking, best practice identification and data standardization and analysis with UC’s Center for Health Quality and Innovation (CHQI), the results have begun to pay off. Post-surgical readmissions have decreased, blood utilization has improved and length of stays have decreased.
Looking ahead — a dynamic, competitive environment and moving forward through uncertainty
Actions at the federal level will reduce the number of people who have health insurance, placing an additional financial strain on the limited resources of public hospitals. Essential programs are under review at federal and state levels, potentially scaling back their scope or redirecting badly needed funds away from safety net hospitals.
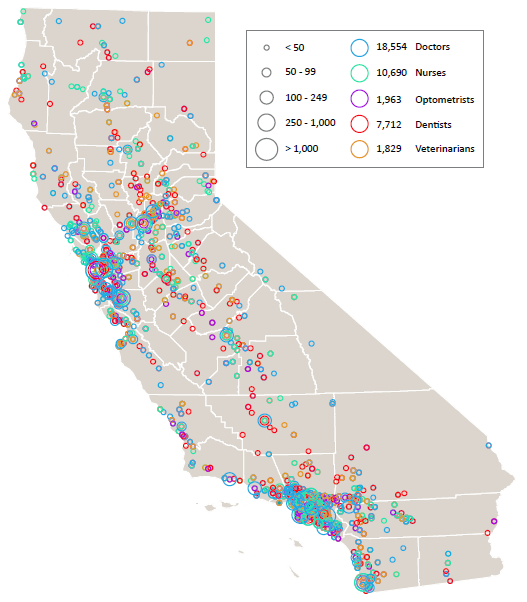
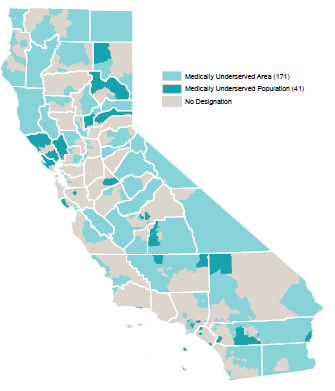
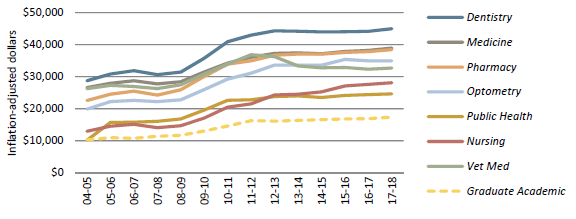
At the same time, California’s population continues to climb. Yet UC’s ability to meet the state’s growing health care needs is hampered. Federal caps on the number of Graduate Medical Education residencies are a bottleneck to growing the number of physicians. Similarly, the ability to train tomorrow’s nurses, optometrists, dentists, pharmacists, public health professionals and veterinarians is constrained by limited state support.
In August 2017, UC President Janet Napolitano, president of the UC system, and Lloyd Dean, president and CEO of Dignity Health, began co-chairing the California Future Health Workforce Commission to bring together policymakers, health care providers, educators and state and community leaders to develop recommendations for legislative and regulatory consideration. For the people of UC Health our three missions continue: educate and train the next generation of caregivers, develop new treatments and cures, and provide a public service to the people of California.
For more information