Health expertise in service of three missions
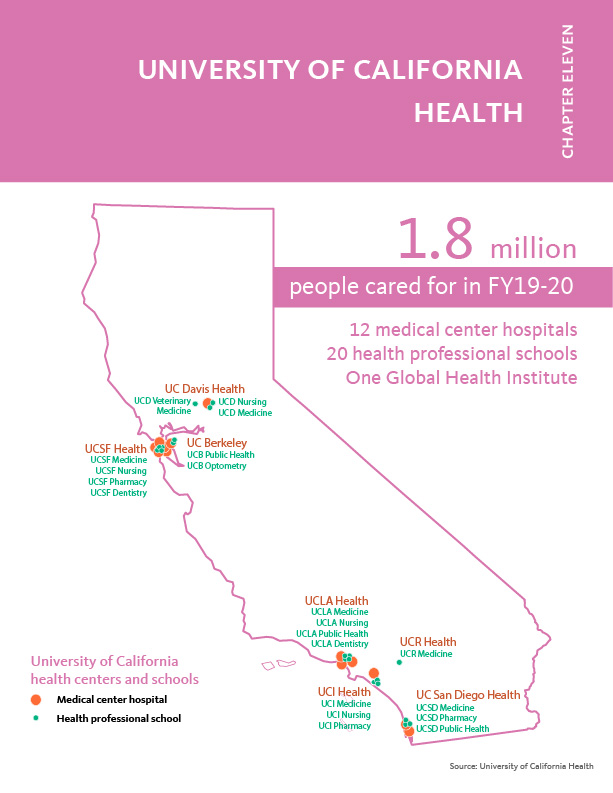
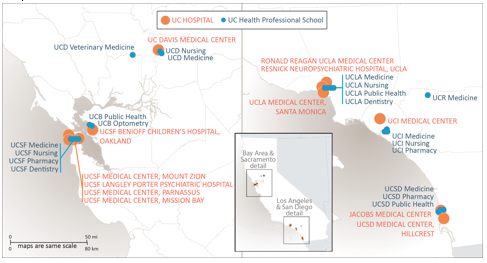
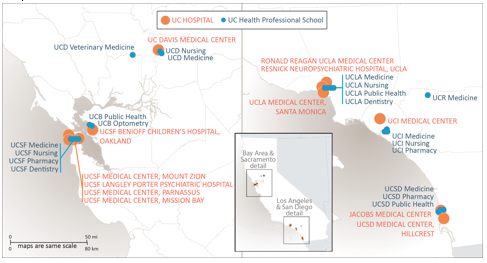
The University’s twenty health professional schools, six academic health systems, student health centers, and self‐funded health plans — collectively referred to a University of California Health (UCH) — are connected and coordinated through the health division office within the UC Office of the President (UCOP).
The health division office facilitates select systemwide activities, provides a long-term strategic framework, and acts as a catalyst for change to ensure the nation’s largest academic health system remains at the forefront of clinical, educational, and research excellence.
A responsive, resilient, and strategic framework
The University’s tripartite mission of teaching, research, and public service informs the UCH five-year strategic plan, which is reviewed annually to ensure it addresses changes in the external environment and proactively captures emerging opportunities. This annual refresh is executed through a collaborative process involving multiple stakeholders, including chancellors, medical center CEOs, deans of the health professional schools, UCOP leadership, and division office leadership. Inherent within this collaborative approach is an acknowledgment that local leadership must remain able to respond to the differing needs of communities, employees, faculty, and students at each location.
The resilience of this approach was demonstrated throughout 2020 and into 2021 as UCH vigorously responded to the COVID-19 pandemic. Under the leadership of Executive Vice President Carrie L. Byington, M.D., a pediatrician, and infectious disease expert, UCH convened experts from across the academic and clinical enterprise to form the UCH Coordinating Committee. Organized into workgroups to address specific challenges, the Committee’s insights provided the foundation for consistent systemwide response and guidance to the University’s Management Response Team and campus leadership for the safe operation of UC’s ten campuses. Even as UCH met the challenges of the pandemic, it also made progress on several strategic goals, including strengthening data analytics, quality and population health initiatives, and the Leveraging Scale for Value program.
Driven by mission, vision, and values
UCH’s mission is to improve the health of all people living in California now and in the future, promote health equity through the elimination of health disparities, and reduce barriers to access to clinical, educational, and research programs by creating more inclusive opportunities for employees, students, and trainees.
The vision is appropriately expansive for an academic health system of its caliber and boldness: the University of California Health will be the pre-eminent, data-driven, learning health care system that improves the human condition. Its actions are rooted in core values of accountability, collaboration, diversity and inclusion, excellence, integrity, innovation, and being mission-driven. This commitment is demonstrated in many ways, including the $1.4 billion in community benefit in FY 19/20 provided by the hospitals operated by UC.
These foundational elements also guided UCH’s response to the pandemic, which confronted the system and its personnel in multiple ways.
The impact of COVID-19 on the health enterprise
The pandemic is not a single challenge, but a series of challenges requiring continual adjustments.
What started in January 2020 as a systemwide preparation for a potential pandemic has evolved month by month. In February 2020, we cared for some of the first patients in the U.S. with COVID-19. What started with a half-dozen inpatients grew to 8,016 inpatients by the end of March 2021. The acute shortages of personal protective equipment (PPE) that marked the earliest phase of the pandemic, and were met by an outpouring of community donations, evolved into spot shortages of vaccines a year later. UCH labs that developed in-house tests for SARS-CoV-2 and were capable of running a few hundred tests a day scaled up to complete 547,458 tests for UCH patients a year later. Plus, the labs also processed more than 500,000 tests for UC students and employees by the fall of 2020, and a nearly equivalent number to help public health agencies, nursing homes, and other systems.
The State of California called upon the University, too. Seeing the impact on hospitals around the world — and then in New York City — Governor Gavin Newsom asked all hospitals in California to increase surge capacity to 40 percent of each facility’s licensed beds. At UCH, that meant rapidly reconfiguring non-clinical space into treatment areas, creating 1,481 beds in surge capacity. We created new beds in every hospital location, including setting up a field hospital at UCI Medical Center in December 2020. When the state realized the scope of infection was overwhelming existing contact-tracing capabilities, UCH launched rapid-training programs that added more than 10,000 contact tracers to the effort. When the state’s public health department was inundated with disparate streams of data, UCH’s Center for Data-driven Insights and Innovations helped harmonize the data to reveal useful patterns enabling data-driven decision and policy making.
Academic health systems are known for innovation and developing new technologies and applications. Here too, UC and UCH rose to the challenge. Early in the pandemic, UCOP responded to more than 300 research proposals by providing micro-grants to jumpstart major initiatives. Dozens of clinical trials were launched, taking a multi-prong approach to exploring new therapeutics, repurposing known drugs, and supporting every COVID-19 vaccine clinical trial conducted in the U.S. UCH physicians tapped into the capabilities of smartphones to set up a Bluetooth-enabled exposure notification system that was rolled out statewide with ten million activations. A breakthrough pooled-testing technology, SwabSeq, expanded the number of samples that could be tested simultaneously while retaining the ability to identify the one positive individual within the sample.
The journey of the pandemic was documented in a series of 30 COVID-19 updates to the Regents from March 2020 through April 2021, as well as year-in-review summaries on UniversityofCalifornia.edu. The number of innovations and extraordinary efforts go beyond what can be captured in this report.
Telehealth evolves into virtual care
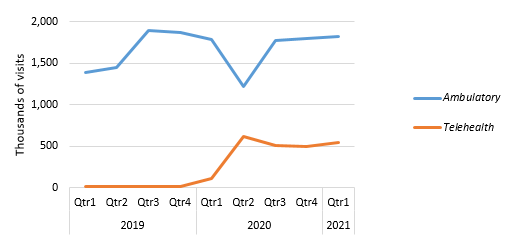
When the pandemic made people reluctant to seek in-person care, telehealth rapidly evolved into virtual care. This included direct-to-patient care between clinician and patient, plus it served as a means of extending UC’s clinical expertise to physicians in emergency rooms and intensive care units at smaller hospitals inundated with COVID-19 patients but lacking needed specialists.
From February 2020 through March of 2021, the direct-to-patient support model went from a systemwide average of 6,000 visits per month to an average of 137,000 per month. This rapid growth exposed patients and clinicians to the matured capabilities of virtual care, overcoming one of the historic barriers to adoption. Even as in-person visits rebound, we believe the landscape is fundamentally more receptive to virtual care, and we are strengthening our infrastructure to leverage virtual care capabilities across a broader array of settings.
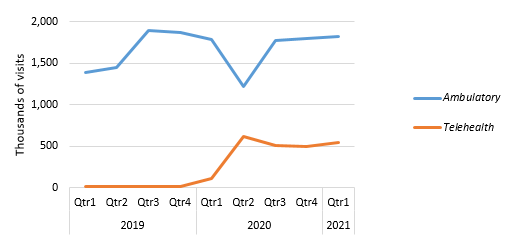
Source: UCH Data Warehouse
Preparing the next generation of health care professionals
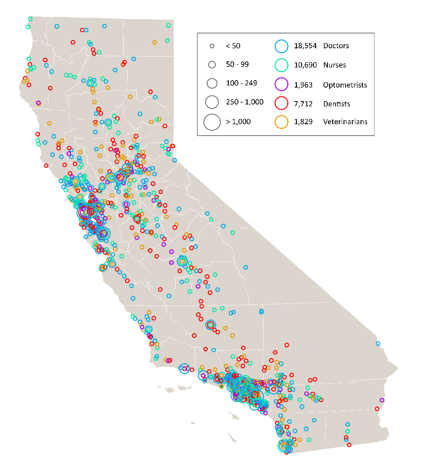
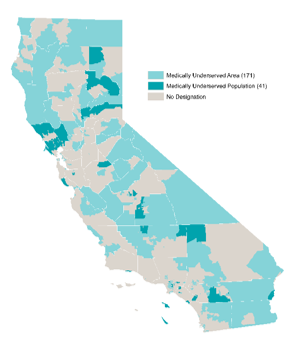
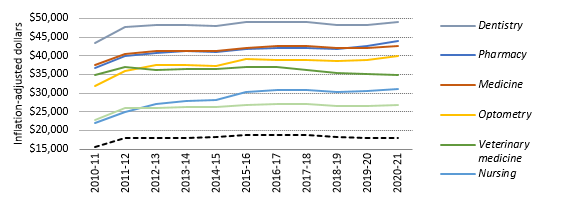
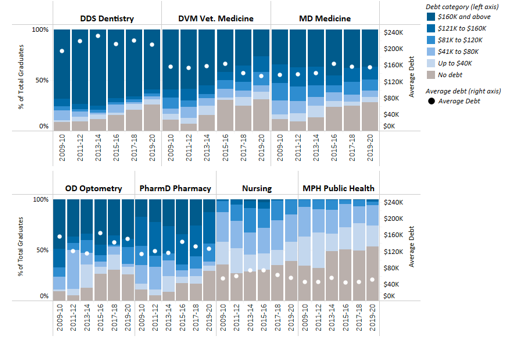
California’s 40 million people need access to care, now and in the future. The state’s growing population is increasingly diverse, growing older, and facing myriad health needs. While some geographic areas have a sufficient supply of health providers, other parts of the state, such as the San Joaquin Valley and Inland Empire, have far fewer health professionals than needed.
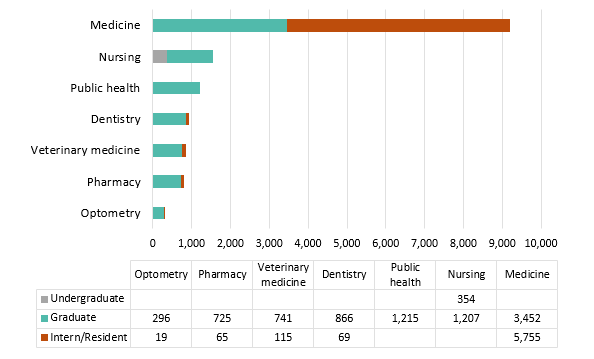
UC’s health sciences programs are a vital source of the state’s future dentists, doctors, nurses, optometrists, pharmacists, public health professionals, and veterinarians. The University is the largest and one of the most comprehensive health sciences training programs in the nation, with nearly 15,000 students. Based on historical averages, more than 70 percent of graduates from these programs will remain in California after graduation or residency.
University of California Health’s 20 health sciences schools are:
- Dentistry (UCSF, UCLA)
- Medicine (UCD, UCSF, UCLA, UCR, UCI, UCSD)
- Nursing (UCD, UCSF, UCLA, UCI)
- Optometry (UCB)
- Pharmacy (UCSF, UCSD, UCI)
- Public Health (UCB, UCLA, UCSD)
- Veterinary Medicine (UCD)
The caliber of UC’s health professional programs is demonstrated in the rankings produced by U.S. News & World Report, current as of April 2021.
|
Category
|
UC Berkeley
|
UC
Davis
|
UC
Irvine
|
UCLA
|
UC
San Diego
|
UC Riverside
|
UCSF
|
|
Best Medical Schools – Research
|
--
|
48 (tie)
|
48 (tie)
|
21
|
19
|
93-123***
|
4
|
|
Best Medical Schools – Primary Care
|
--
|
11
|
41
|
12
|
28
|
93-123***
|
2
|
|
Best Nursing Schools – Masters
|
--
|
24
|
45
|
16
|
--
|
--
|
9
|
|
Best Graduate Schools Public Health
|
8
|
24*
|
41*
|
10
|
--
|
--
|
--
|
|
Best Pharmacy Schools**
|
--
|
--
|
--
|
--
|
18
|
--
|
2
|
|
Best Veterinary Medicine Schools**
|
--
|
1
|
--
|
--
|
--
|
--
|
--
|
* Indicates a degree program rather than a school.
** Indicates these graduate schools were ranked in previous years and remain current as of publication date. USN&WR does not rank dental or optometry programs.
*** Indicates a grouped ranking.
In 2021, US News & World Report added a new diversity ranking for medical schools. Four of the six UC medical schools are among the top ten in the nation for diversity.
National Rankings of Medical Schools Based on Diversity
- #4 UC Davis SOM
- #6 UC Riverside SOM
- #9 UCLA DGSOM (tie)
- #9 UCSF SOM (tie)
To make progress toward health equity, we must have health care providers who reflect the diversity of our communities. Following four years of medical school, graduates then enter another period of training — Graduate Medical Education (GME). In May 2021, UC medical school graduates had a ‘match rate’ of 98.3 percent into GME residency programs and of those, 42 percent matched at a UC hospital. This demonstrates the integral relationship between health education and health care delivery.
GME programs provide in-depth training that may last three to seven years depending on the specialization. All of UC’s academic health centers provide residency programs and fund a substantial number of them without traditional federal support. In the 1960s, Medicare began paying for a substantial portion of the cost of residency programs. In 1997, it limited the number of funded residencies. The cap on Medicare-funded residencies has not been revised upward since then, despite a growing and aging national population with more health care needs. As a result, UC academic health centers began absorbing costs for residency training positions. In 2019–20, UCH trained 5,708 medical residents. Of those, 839 positions receive no direct federal GME direct support, at a cost of $102 million to the University.
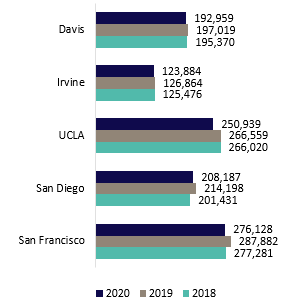
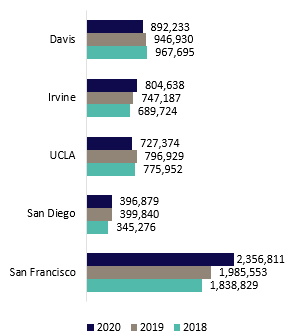
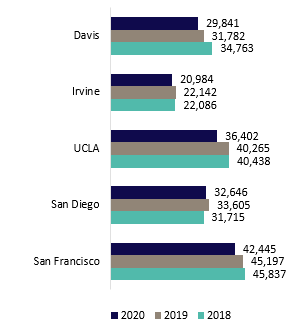
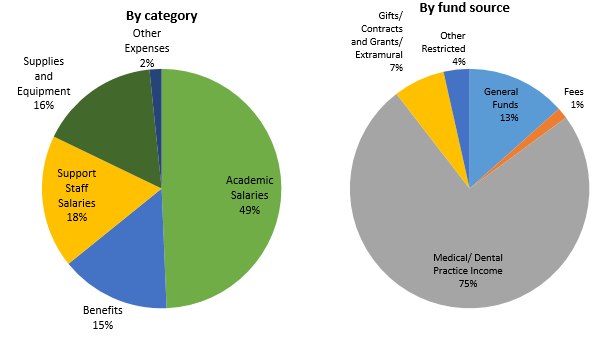
Academic Health Centers
UCH includes six academic health centers, five of which own or operate their hospitals, and one that leverages a community-based training and care delivery platform. The hospitals of UC Davis Health, UCI Health, UCLA Health, UC San Diego Health, and UCSF Health admitted 162,318 patients in FY19/20 for 1,052,097 inpatient days. The hospitals also provided 5,177,935 hospital-based outpatient clinic visits. When combined with outpatient services of the health professional schools, UCH provided nearly 8.2 million outpatient visits and cared for approximately 1.8 million unique patients.
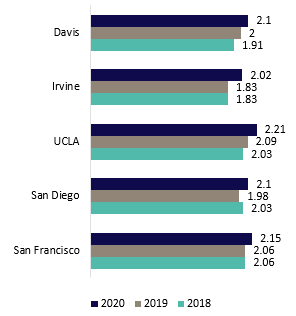
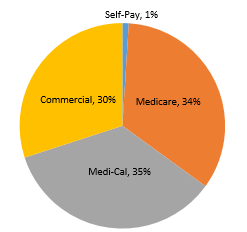
UCH is an essential part of California’s health care safety net system. Care is provided regardless of whether the person has health insurance. The academic health centers are supported almost entirely by reimbursement for clinical services paid by Medi-Cal (Medicaid), Medicare, and commercial payers. Systemwide, in FY19/20, 35.5 percent of inpatient days were associated with Medi-Cal, 34.1 percent with Medicare, and 29.6 percent with private market payers. The remaining 0.7 percent lacked any form of insurance or were self-paid. Statewide, the pandemic has driven a 6.8 percent increase in Medi-Cal enrollment. Although UC hospitals represent less than six percent of the acute care beds in the state, they are the third-largest provider of inpatient services and the fourth-largest provider of hospital-based outpatient services.
Clinical quality is another area of distinction. All five UC academic health centers that own or operate hospitals are ranked among California’s top hospitals and two are on the national honor roll, according to U.S. News & World Report, which has ranked hospitals for more than three decades. The 2020–2021 Best Hospital rankings for UC hospitals are:
Best Hospitals, Nationally
#4 UCLA
#8 UCSF
Best Hospitals, California
#1 UCLA
#3 UCSF
#6 UC San Diego
#9 UC Davis
#11 UCI
UCH also has a significant economic impact on California. A January 2021 report by Beacon Economics noted the University has an $82 billion impact on the state, of which the health enterprise represents $37 billion.
Progress on Systemness
The first move toward ‘systemness’ began with the Leveraging Scale for Value (LSfV) initiative six years ago, which works on supply chain, revenue cycle, and information technology improvements. The program generated $550M in value for FY19–-20 and a cumulative benefit of approximately $1.5 billion since its inception six years ago.
More recently, cross-campus collaborations have expanded to numerous clinical and research programs. By 2021, dozens of active multi-campus collaborations were underway, accelerating the pace of discovery, sharing of best practices, and improved coordination. One such example is CORDS, a database of de-identified clinical information from COVID-19 patients across the UCH system, which led to 14 peer-reviewed papers, new treatment insights, and a substantial scientific contribution to the National COVID Cohort Collaborative, a program run by the NIH’s National Center for Advancing Translational Sciences.
Another example of systemness is a COVID-19 dashboard that leverages all five instances of UC’s electronic health record platform. The dashboard shows the SARS-CoV-2 tests performed each day for UCH patients, the positive tests by gender, age, and geography, the inpatients with a COVID-19 diagnosis with details on ICU and ventilator use, and the disposition of patients at the end of treatment. These metrics are reported via UCH’s Twitter account (@UofCAHealth).
As noted in the vision statement, UCH intends to be the ‘pre-eminent data-driven learning healthcare system,’ and its ability to rapidly leverage information from the UCH Data Warehouse is a sample of what can be accomplished.
For more information
University of California Health
University of California Health impact
UC Budget for Current Operations, 2021-22
UC-trained health professionals in California
Medical Centers Annual Financial Report
More University of California Health reports and resources