Health expertise in service of three missions
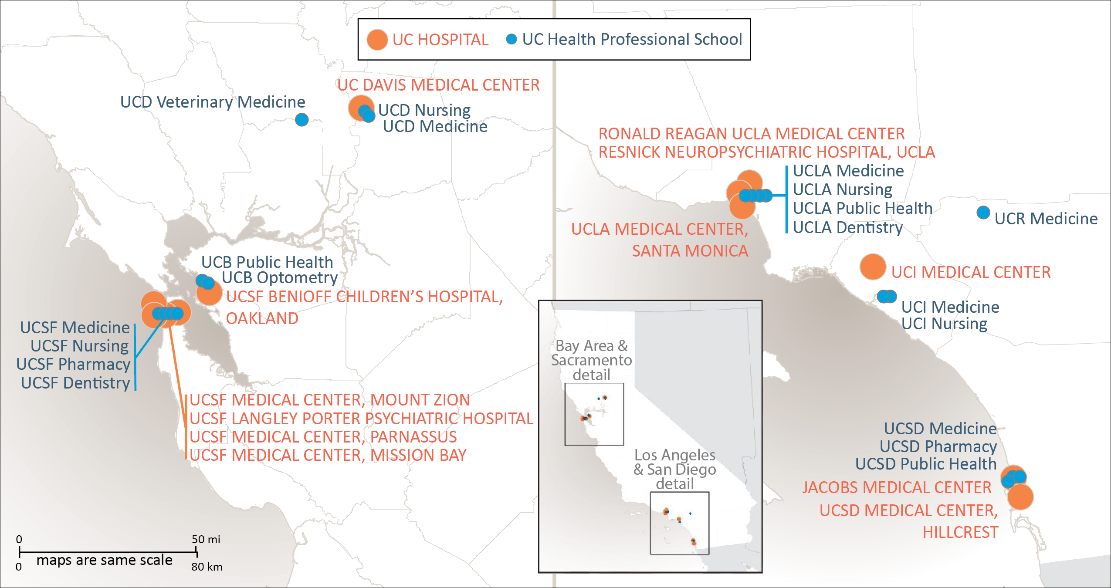
The University’s 19 health sciences schools, six health systems, student health centers, and self‐funded health plans are connected by UC Health, the division office within the Office of the President. The activities of the division, and the broader health enterprise, are aligned to support the University’s tripartite mission of teaching, research, and public service.
A refreshed strategic framework and new leadership
The strategic plan for the division office of UC Health was developed in December, 2017 and is refined annually based on feedback from stakeholders, including chancellors, medical center CEOs, deans of the health professional schools, UCOP leadership, and UC Health department heads. UC Health's strategic plan also aligns with the strategic framework of UCOP.
An update completed in January, 2020 also reflects the new leadership of UC Health. On October 31, 2019, Dr. Carrie L. Byington, a physician-scientist, pediatrician, and internationally recognized infectious disease expert, became executive vice president of UC Health, succeeding Dr. John D. Stobo, who led the division since 2008.
The UC Health division office functions as a catalyst for change, coordinating various systemwide activities and providing a strategic framework while respecting the need for local leadership in responding to the needs of their communities, employees, faculty, and students.
The 2020 strategic plan outlines 13 goals to set the direction through 2022. This multi-year framework also sets in motion collaborative efforts that draw upon academic, research, and clinical capabilities across the University's enterprise. As a “living document,” the strategic plan anticipates and provides flexibility within broad market forces that include changes in reimbursement from governmental and commercial payers, evolving demographics of the state, changes in drug prices, the impact of climate change on health, and expectations for improved management of chronic conditions, including the opioid epidemic.
At the time of the plan’s development, the outbreak of novel coronavirus (SARS-CoV-2) was in its earliest stages, and its spread within the U.S., and its impact on all health systems, not yet realized. Given the unprecedented scale of the COVID-19 pandemic, UC Health and the University of California are responding with the full scope of their patient care, education and training, and research capabilities. The division will continue to drive progress towards its strategic goals within the context of the broader public health threat of COVID-19.
Mission, vision, and values
UC Health’s mission is to improve the health of all people living in California now and in the future, promote health equity through the elimination of health disparities, and reduce barriers to access to clinical, educational, and research programs by creating more inclusive opportunities for employees, students, and trainees.
The vision is expansive; UC Health’s collaborative approach will be recognized as the foundation for building the pre-eminent data-driven learning healthcare system that improves the human condition. Its actions are rooted in core values of accountability, collaboration, diversity and inclusion, excellence, integrity, innovation and being mission-driven. UC Health’s mission, vision, and values are appropriately ambitious for an academic health system committed to the health of California and reflect the spirit of being ‘Boldly Californian.’
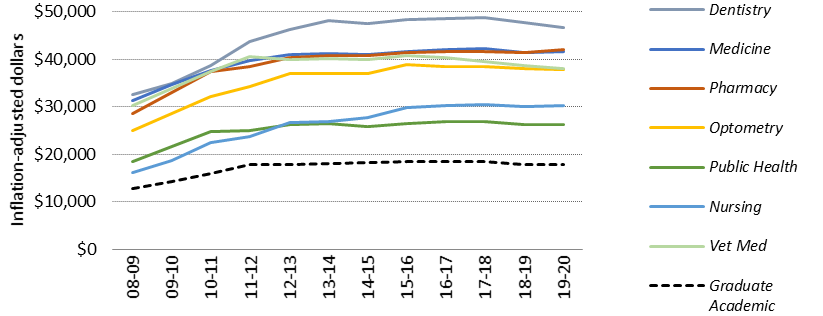
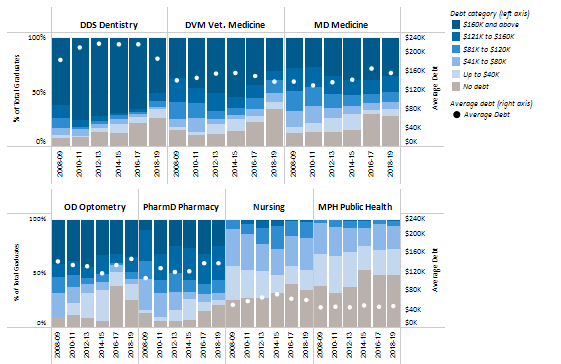
Preparing the next generation of health care professionals
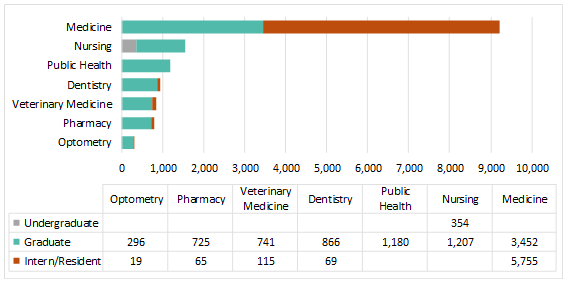
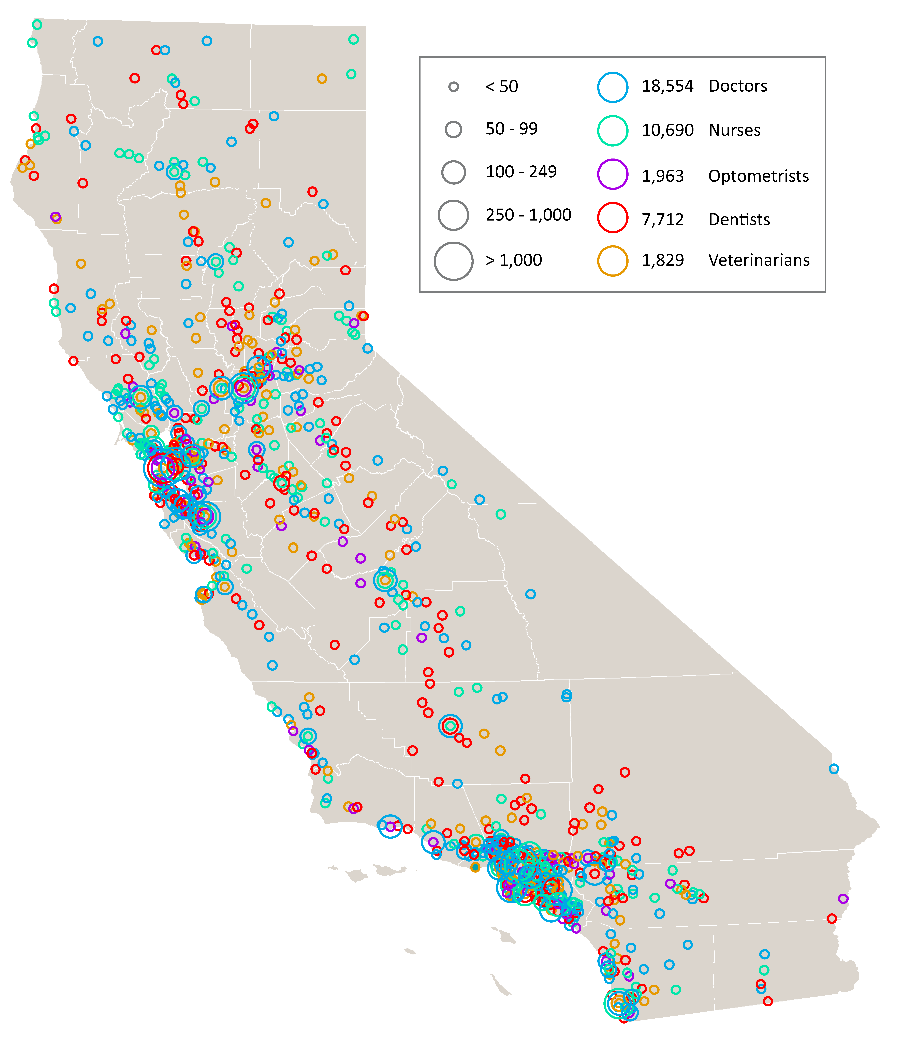
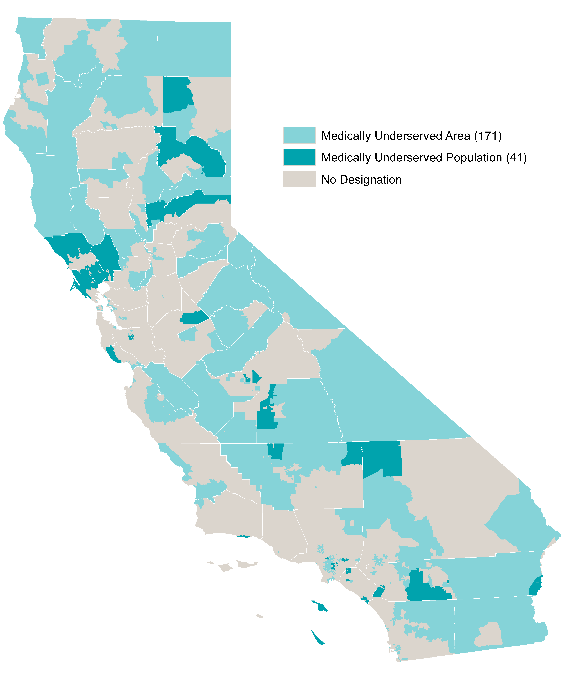
California’s 40 million people need access to care, now and in the future. The state’s growing population is increasingly diverse, growing older, and faces myriad health needs. While some geographic areas have a sufficient supply of health providers, other parts of the state, such as the San Joaquin Valley and Inland Empire, have far fewer health professionals than needed. UC’s health sciences programs are a vital source of the state’s future dentists, doctors, nurses, optometrists, pharmacists, public health professionals, and veterinarians. The University is the largest and one of the most comprehensive health sciences training programs in the nation, with nearly 15,000 students. Based on historical averages, more than 70 percent of graduates from these programs will remain in California after graduation or residency.
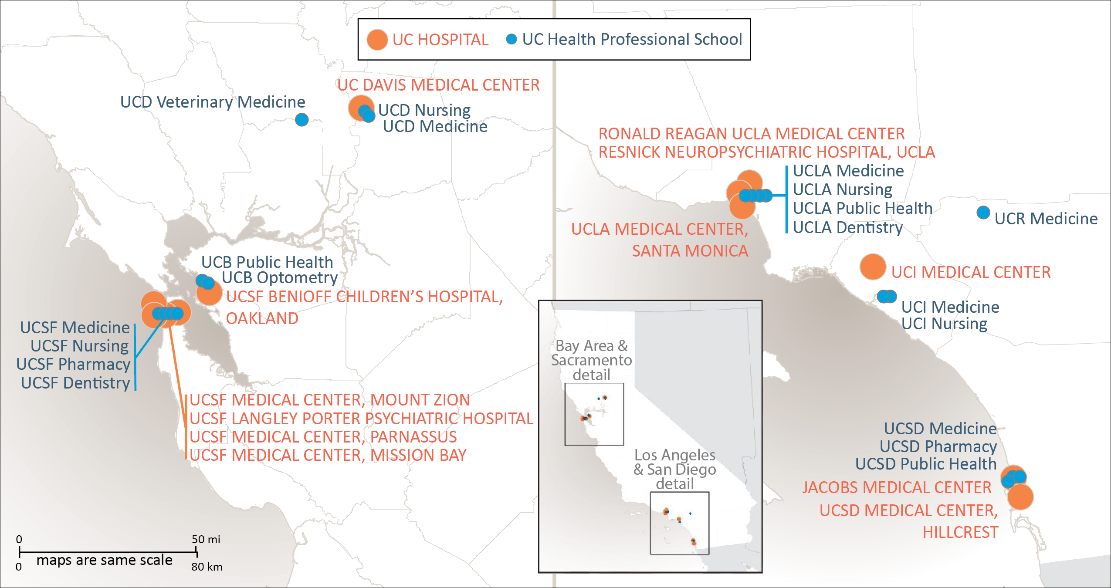
UC Health’s 19 health sciences schools are:
- Dentistry (UCSF, UCLA)
- Medicine (UCD, UCSF, UCLA, UCR, UCI, UCSD)
- Nursing (UCD, UCSF, UCLA, UCI)
- Optometry (UCB)
- Pharmacy (UCSF, UCSD)
- Public Health (UCB, UCLA, UCSD)
- Veterinary Medicine (UCD)
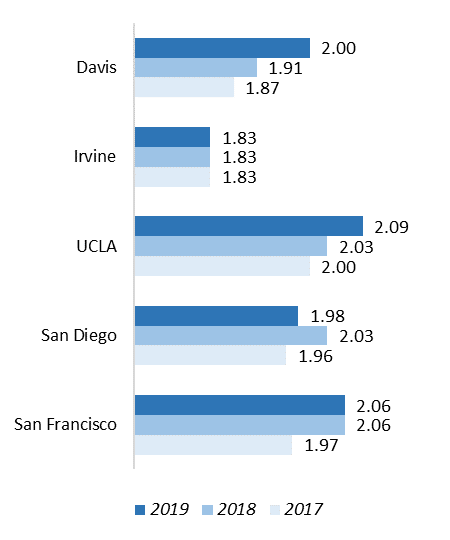
The caliber of UC health professional programs is demonstrated in the rankings produced by U.S. News & World Report, shown below as of 2019-2020:
|
Category
|
UC Berkeley
|
UC
Davis
|
UC
Irvine
|
UCLA
|
UC
San Diego
|
UC Riverside
|
UCSF
|
|
Best Medical Schools – Research*
|
--
|
40
|
44
|
6 (tie)
|
21
|
91
|
6 (tie)
|
|
Best Medical Schools – Primary Care*
|
--
|
7
|
81
|
11
|
26
|
92
|
2
|
|
Best Nursing Schools – Masters*
|
--
|
40
|
51
|
20
|
--
|
--
|
11
|
|
Best Graduate Schools Public Health
|
9
|
--
|
--
|
11
|
--
|
--
|
--
|
|
Best Pharmacy Schools*
|
--
|
--
|
--
|
--
|
18
|
--
|
2
|
|
Best Veterinary Medicine Schools
|
--
|
1
|
--
|
--
|
--
|
--
|
--
|
* Indicates 2020–2021 update by U.S. News & World Report. All others based on 2019–2020 rankings. USN&WR does not rank dental or optometry programs.
Academic Health Systems
UC Health includes six academic health centers (AHCs), five of which own or operate their hospitals, and one that leverages a community-based training and care delivery platform. The hospitals of UC Davis Health, UCI Health, UCLA Health, UC San Diego Health, and UCSF Health admitted 172,991 patients in FY18/19 for a total of 1,092,522 inpatient days. The hospitals also provided 4,876,439 hospital-based outpatient clinic visits. When combined with outpatient services of the health professional schools, UC Health provided more than 7.6 million outpatient visits and cared for 1.8 million unique patients in the most recent fiscal year.
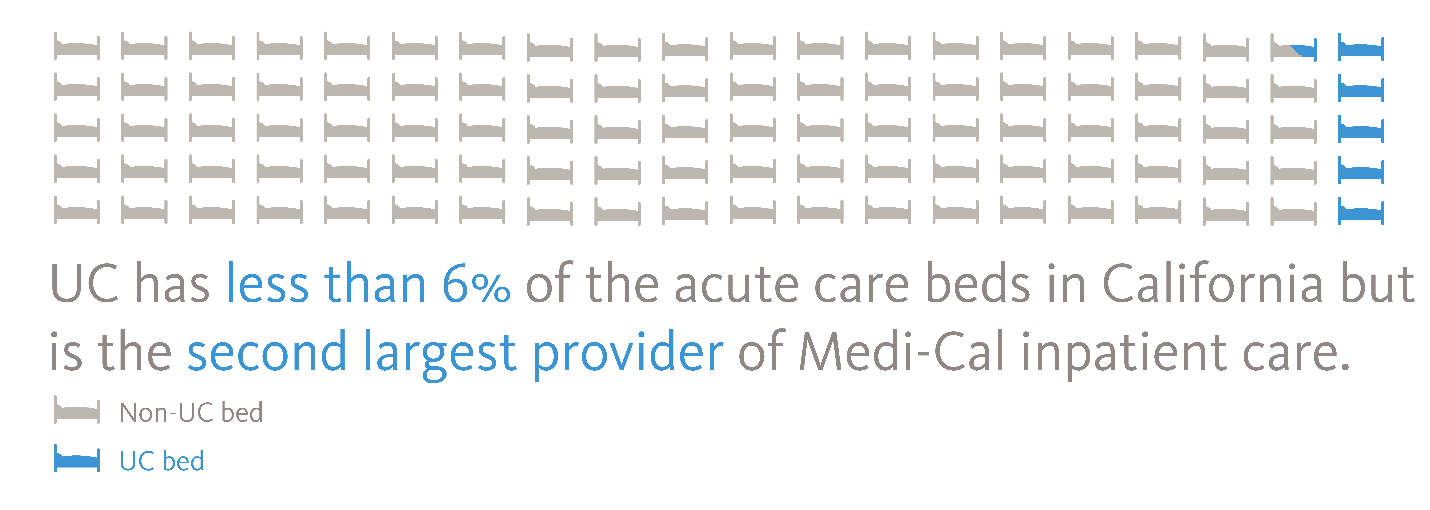
UC health systems are part of the backbone of California's safety net for health care. Care is provided regardless of whether the person has health insurance. The medical centers are supported almost entirely by reimbursement for clinical services paid by Medi-Cal (Medicaid), Medicare, and commercial payers. Systemwide, in FY18/19, 35 percent of inpatient days were associated with Medi-Cal, 34 percent with Medicare, and 30 percent with private market payers. The remaining 1 percent lacked any form of insurance or were self-paid. Almost one in three Californians — 13.5 million people — have health insurance coverage through Medi‐Cal.Although UC hospitals represent less than six percent of the acute care beds in the state, they are the third-largest provider of inpatient services and the fourth-largest provider of hospital-based outpatient services. The number of people eligible for Medi-Cal may expand as the economic fallout from the pandemic continues.
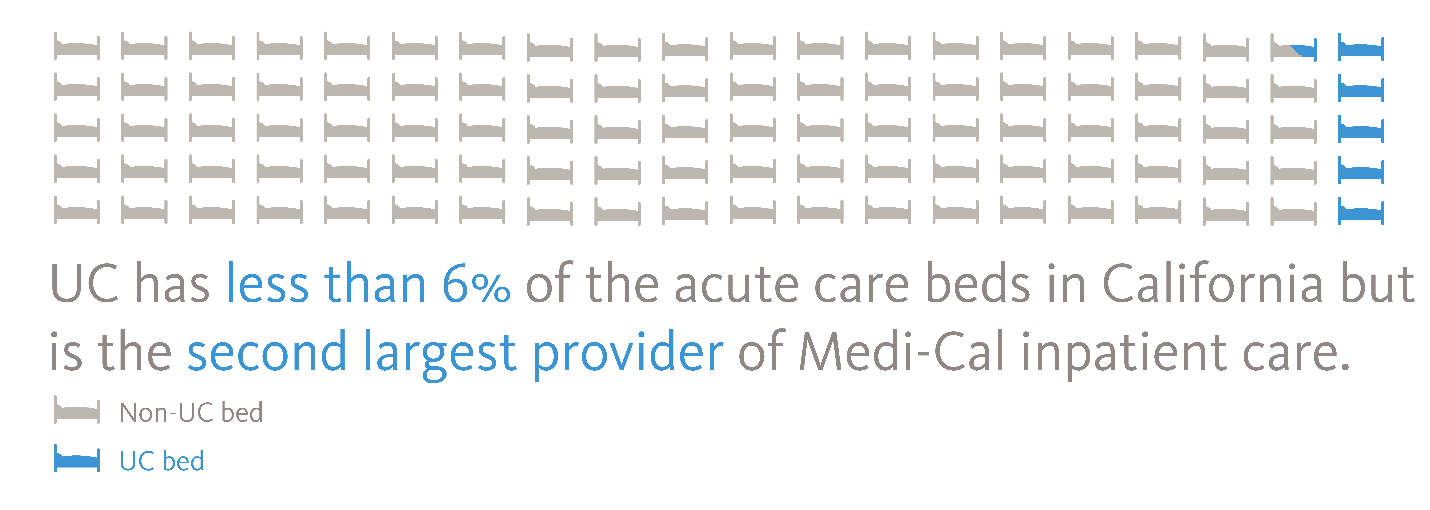
Source: American Hospital Directory cites 74,925 non-federal, short-term, acute care staffed hospital beds in CA.
All five UC medical centers are ranked among California’s top ten hospitals and two are on the national honor roll, according to U.S. News & World Report, which has ranked hospitals for more than three decades. The 2019–2020 Best Hospital rankings for UC hospitals are:
Best Hospitals - Nationally
#6 UCSF
#7 UCLA
Best Hospitals - California
#1 UCLA
#2 UCSF
#6 UC Davis
#8 UC San Diego
#10 (tie) UCI
Leveraging Scale for Value (LSfV)
One of the earliest systemwide collaborations is the Leveraging Scale for Value initiative (LSfV), which works on supply chain, revenue cycle, and information technology improvements. The cumulative financial benefit for this project is more than $950 million as of FY18/19.
The impact of Covid-19 on the health enterprise
In late 2019, China experienced an outbreak of a new virus, initially referred to as ‘2019-nCoV,’ or ‘novel coronavirus’ and ultimately designated ‘SARS-CoV-2.’ The illness it produces is called COVID-19. The World Health Organization (WHO) declared a Public Health Emergency of International Concern on January 30, 2020, and subsequently a pandemic on March 11, 2020. Within months, the world witnessed one competent health system after another become overwhelmed with patients in acute respiratory distress and a high mortality rate.
To support the University’s response, the health division established the UC Health Coordinating Committee and formed working groups of subject matter experts. Among the immediate challenges was a disruption to the global supply chain for Personal Protective Equipment (PPE), which is disproportionately made in China, where manufacturing operations had been suspended.
By late February, UC medical centers had cared for six patients confirmed to have COVID-19, and another 31 whose tests results were pending. Two months later, more than 600 inpatients with COVID-19 had been cared for at UC hospitals. In January and February 2020, there was a national shortage of reliable, mass-produced tests capable of rapidly detecting the virus. Widespread testing is a cornerstone of calibrating infectious disease response based on an understanding of how far the virus has spread, its rate of transmission, and the percent of infected persons who will require hospitalization and ventilation support.
In late February, the Food and Drug Administration permitted sophisticated non-federal labs to independently develop and use tests. By March 10, several UC medical centers had begun in-house testing, and by mid-March, all UC medical centers had the capacity to test with a faster turn-around time than was possible through tests shipped to the CDC. A little more than a month later, more than 35,000 tests had been performed for UC Health patients, and an equivalent number conducted for other hospitals and public health departments.
On March 4, Governor Newsom declared a state of emergency to strengthen the state’s response to the pandemic. UC hospitals had already begun implementing emergency operations plans, ultimately adding 1,481 surge beds to the existing 3,911 beds, an increase of nearly 40 percent.
UC and its health enterprise also responded with accelerated research initiatives. By early April, more than 300 research projects, proposals and clinical trials for COVID-19 were active, and the University had begun distributing initial grants to jump-start efforts.
The pandemic’s threat to health and safety continues, as does its mounting financial toll. UC Health’s medical centers are incurring substantial costs for surge expansion, surge staffing, development of testing capabilities, and other expenses. At the same time, revenues are down due to the cancellation of thousands of non-emergency procedures to prepare for a potential COVID-19 patient surge.
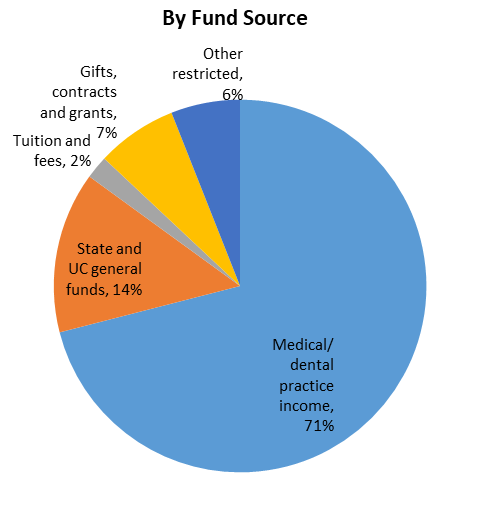
Although the federal government has implemented a series of stimulus bills that will provide some relief, the extent of available funds and how it compares to the expenses and lost revenue will not be known for some time. This is significant as the revenue generated by UC’s clinical activities also support the health professional schools. In FY 18/19, the health services support totaled $606 million.
The economic disruption caused by COVID-19 is enormous. As people lose employer-sponsored health insurance, the people transitioning to Medi-Cal or becoming uninsured will have a direct impact on the payer mix and total revenue received by the medical centers.
Progress on Systemness
The first move toward ‘systemness’ began five years ago, through the Leveraging Scale for Value (LSfV) initiative. By 2019, there were more than a dozen collaborations across the system sharing best practices and coordinating activities. Today, as a result of COVID-19, that number has grown significantly.
One sign of this effort is a COVID-19 dashboard that leverages all five instances of UC’s electronic health record platform. The dashboard shows the SARS-CoV-2 tests performed each day for UC Health patients, the positive tests by gender, age and geography, the inpatients with a COVID-19 diagnosis with details on ICU and ventilator use, and the disposition of patients at the end of treatment. These metrics are reported via UC Health’s Twitter account (@UofCAHealth). As noted in the vision statement, UC Health intends to be the ‘pre-eminent data-driven learning healthcare system,’ and its ability to rapidly leverage information from the UC Health Data Warehouse is a sample of what can be accomplished.
In April, the Robert Wood Johnson Foundation, the country’s largest philanthropic foundation focused solely on health, awarded UC Health a $100,000 grant to work with other health systems to increase the availability of standardized, actionable information on COVID-19 impact and progression.
For more information