On the evening of Nov. 10, the School of Medicine held their inaugural American Indian Medical Student Blessing Ceremony and Blanket Presentation. Blanket ceremonies are a pan-Indigenous practice that celebrate individuals going through life-changing events. On this night, eight Native American medical students would be recognized for their growing contributions to the community, as they transitioned from students to student-doctors.
This ceremony is the latest in a series of recent initiatives by the School of Medicine to promote Native American recruitment, retention and educational programming. A sense of community pride was shared amongst the Native students, staff, faculty and local representatives in the crowd.
The night began by addressing the university’s role as a land grant institution. UC San Diego was built on the unceded territory of the Kumeyaay Nation, whose people remain a vital part of the local community. San Diego County also has the highest number of Tribal Nations in the country, but still only 1 percent of UC San Diego medical students identify as American Indian or Alaska Native.
“Being a land grant institution gives you a responsibility to serve not just Tribal communities on that land, but across the entire country,” said Alec Calac, a public health MD/PhD student and member of the Pauma Band of Luiseño Indians, a local Tribe in San Diego County. “As the region's only academic medical center, we have an affirmative obligation to educate Tribal members. I think UC San Diego has done a lot of honest introspection on this in recent years, and the presence of these eight students shows we’ve come a long way.”
improving health and well-being for all
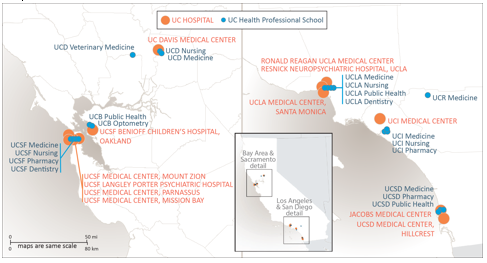
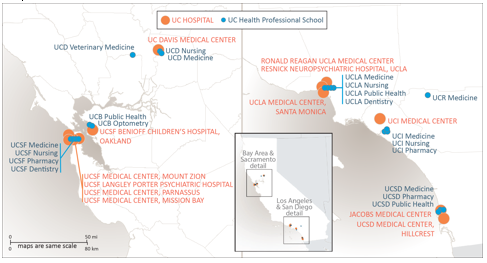
Health is a crucial concern in all California communities, and we are facing many challenges – from deadly viruses and accelerating climate change to global conflict and migration. Guided by its tripartite mission of teaching, research, and public service, the University of California has a bold vision: to improve the health and well-being of all people living in California now and in the future by better educating and training the inclusive workforce of tomorrow; delivering exceptional care; and discovering life-changing treatments and cures. This expansive aim is appropriate for the University of California, which is home to the country’s largest academic health system comprising 20 health professional schools, six academic health centers, ten student health centers, the systemwide Global Health Institute, and self‐funded health plans.
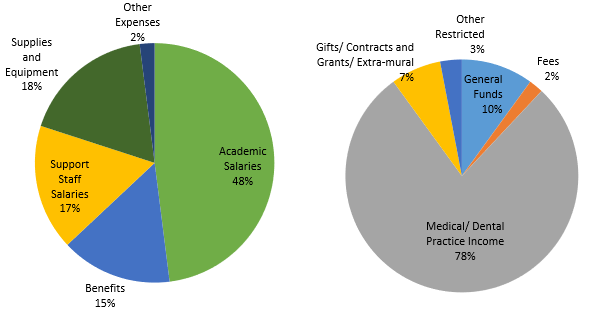
The health division within the UC Office of the President connects the people and resources of the health enterprise and coordinates key systemwide activities where the power of UC’s health expertise and resources working together adds value. Initiatives flow from a long-term strategic framework to keep the system at the forefront of clinical, educational, and research excellence. Among the top priorities are promoting health equity through the elimination of health disparities, and creation of more inclusive opportunities for students, faculty, and employees. The vision for the health system also centers on ensuring it is a data-driven, learning, health care organization achieving excellence across all of its functions. Operationally, the health division also focuses on identifying opportunities to achieve economies of scale for the system. The systemwide Leveraging Scale for Value program generated $204M in value for FY 2021 and has delivered a cumulative benefit of approximately $1.7 billion since its inception.
The outcomes of the University’s commitment to improving health and well-being for all are demonstrated in many ways, including through $3.9B in community benefits delivered by UC’s academic health centers and faculty practices in FY 2020.
learning and adapting for what's ahead
Experiences during the past several years have cast a brighter light on the realities and impact of health disparities, climate change, and migration on the human condition. UC’s health care delivery, education, and research teams have demonstrated their resiliency during these difficult times and now are embracing and acting on lessons collectively learned. Initiatives have begun addressing urgent issues that will surely dominate the health field during the years to come.
The critical role of data in the pursuit of improved health equity became apparent during the pandemic. COVID-19 has disrupted lives, interrupted health maintenance and care, and further highlighted existing health disparities. To improve health equity, systemwide efforts are leveraging advancements made in data gathering, integration, and modeling by the Center for Data-driven Insights and Innovation that were critical for the COVID-19 response. Data sets integrating information from UC’s six academic health centers and faculty practices have been analyzed and categorized using state and national indices including the California Healthy Places Index, the Social Vulnerability Index, and the Area Deprivation Index, which give a more accurate representation of UC patient demographics. The enhanced data help identify best practices and monitor quality improvement outcomes by social indices, race, and ethnicity. In another example of enhanced data use, the systemwide Quality & Population Health program brought UC’s health services research community together to identify drivers of a disparity in blood pressure for Non-Hispanic Black patients. The drivers will be used to help design improvement work at each academic health center.
The importance of supporting the health of the most vulnerable in our interconnected world was evident as historic numbers of unaccompanied minor children came across the southern border of the United States at the same time as the COVID-19 crisis. UC’s academic health centers mobilized to care for them, supporting the health of these children while also helping mitigate risks from potential COVID-19 spread. A systemwide rapid response brought multi-disciplinary teams of UC child health professionals to two major intake sites in the state, supported by UC resources including laboratory, radiological, and emergency equipment; electronic medical records; medical supplies; pharmaceuticals, and vaccines. During the five-month response in spring 2021, UC teams provided state-of-the-art preventative and interventional care for nearly 5,000 children and adolescents. All children received triage visits on arrival and full exams within 24-48 hours. UC providers were available 24/7 on-site and delivered an additional 11,000 urgent care visits and nearly 8,800 doses of vaccines. Approximately 16 percent of children had COVID-19, most infected prior to arrival. Infection prevention processes prevented forward transmission within the emergency sites or in the community. In addition to medical care, culturally-sensitive psychological, social, and dietary support was extended to all, ensuring availability of trauma-informed care. In addition to being valued by the children, this work enhanced the educational experience for many graduate medical residents and fellows and provided lessons learned for creating culturally sensitive, trauma-informed care.
Climate issues have become one of the most serious threats to health. Accelerating emergence of new viruses, declines in air quality, natural disasters, and food supply disruptions are all among the climate-related impacts that must be addressed by health professionals and systems. For many years, UC has been working to update its health operations to cause less impact on the environment and its communities. Health teams across the system have made progress on sustainability goals and will be using learnings from that work to update systemwide goals and take additional actions. Existing efforts led to the system being named a 2021 Climate Champion by Health Care Without Harm, and all of UC’s academic health centers being recognized by Practice Greenhealth as 2021 Environmental Excellence Award winners. Additionally, a grant from America’s Essential Hospitals is helping share across the system best practices developed at UCSF Health that reduce carbon emissions from anesthesia gases as well as actions for reducing energy consumption in operating rooms.
With these and other learnings in mind, the health division has launched a deep-dive strategic planning process to create the next five-year strategic plan to prioritize the areas where systemwide collaboration can add additional value and ensure ongoing resilience, learning, and excellence.
covid-19 response adn prevention continue
The pandemic continues to impact UC’s health system. UC’s academic health centers have remained on the front lines of response, including caring for patients during the winter 2021–22 surge driven by the omicron variant, with COVID-19 hospitalizations at UC academic health centers reaching a high on January 20, 2022. Since identification of COVID-19 in the State through mid-April 2022, UC hospitals have cared for more than 100,000 patients with COVID-19. Vaccination has been a focus of UC’s prevention work and has included administering more than 1.5 million COVID-19 vaccine doses as of mid-April 2022, including numerous clinics in medically underserved areas working with community partners.
The work in prevention and monitoring also involved enhanced data support as the Center for Data-driven Insights and Innovation created more robust vaccine reporting to the State and expanded data in its regularly published COVID-19 dashboards. This reporting gave public health officials and the public an understanding of the level of community spread of the virus, the burden on hospitals and the outcomes of the robust testing efforts engaged in by UC labs. The data provided evidence-based inputs for decision making by public health authorities as well as for individuals evaluating their own personal risks.
UC’s health experts were equally engaged in informing UC campus response and prevention as detailed in a research study published in November 2021 in PLOS ONE. The mitigation efforts informed by the UC Systemwide COVID-19 Public Health Workgroup to reduce COVID-19 on the ten University of California campuses minimized campus transmission and outbreaks and limited spread to surrounding communities. UC Student Health and Counseling centers served as a pivotal resource in the on-campus COVID-19 pandemic response, allowing the campuses to return to in-person learning in fall 2021. Since the onset of the COVID pandemic, the Student Health and Counseling centers have tracked more than one million doses of COVID-19 vaccine; followed more than two million COVID-19 surveillance tests for students, staff, and faculty; diagnosed more than 13,000 cases of COVID and arranged quarantine and isolation for more than 28,000 students across the system. In addition, Student Health and Counseling centers provided ongoing primary care and behavioral health care via telehealth and medications-by-mail to many of UC’s 294,000 students during this period.
improving access and equity through the next generation of health care professionals
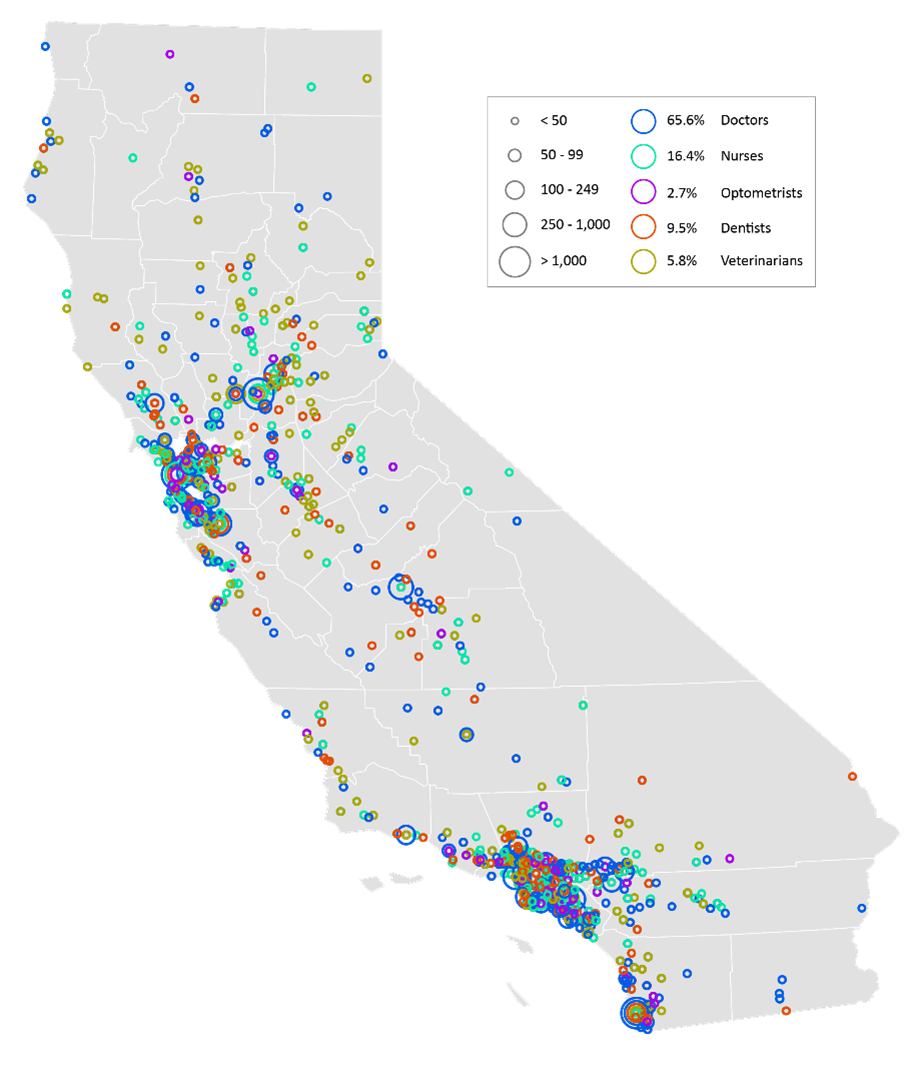
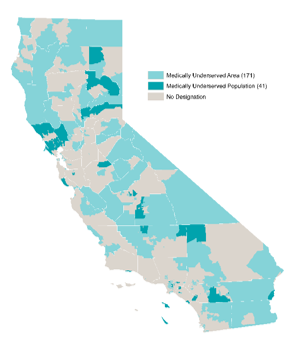
As the most populous state in the nation with nearly 40 million people, California has a critical need to ensure robust access to quality health care. This need will become even greater as the state’s population grows and becomes increasingly diverse and older, while facing myriad health needs. While some geographic areas have a sufficient supply of health providers, other regions in the central part of the state have far fewer health professionals than needed.
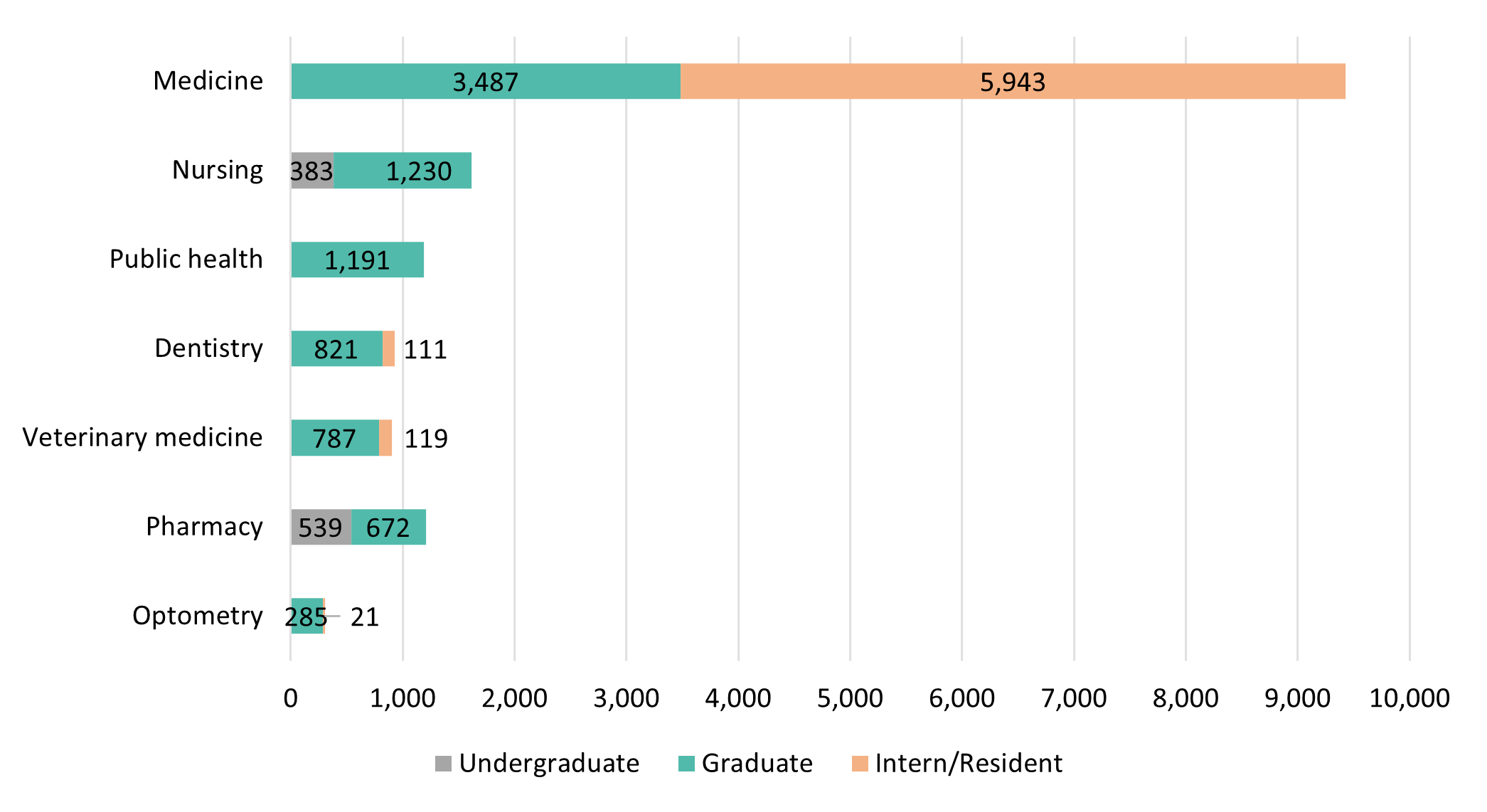
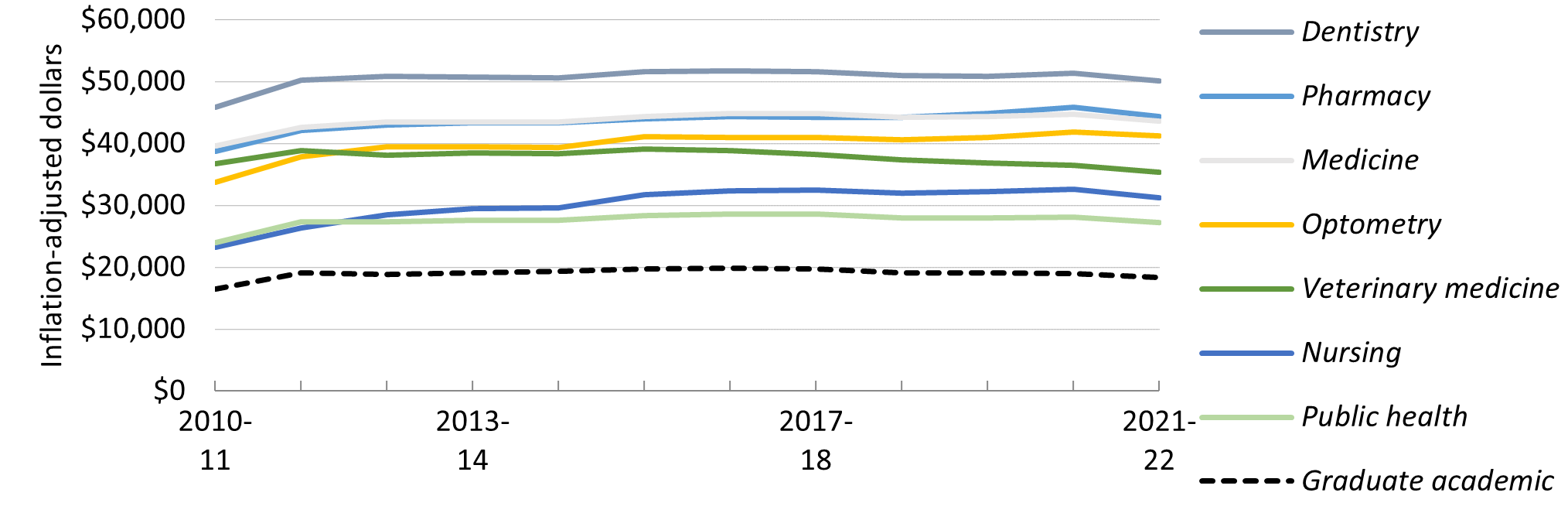
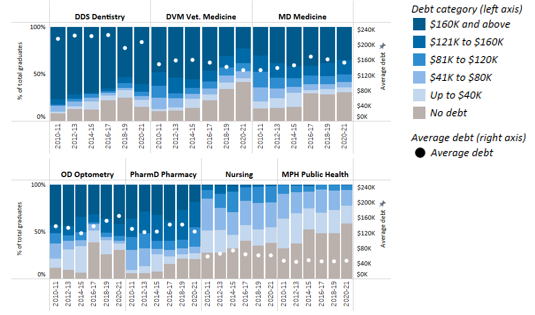
UC’s health sciences programs are a vital source of the state’s future dentists, doctors, nurses, optometrists, pharmacists, public health professionals, and veterinarians. The University is the largest and one of the most comprehensive health sciences training programs in the nation, with over 15,500 students. Based on historical averages, more than 70 percent of graduates from these programs will remain in California after graduation or residency. This high rate of retention reflects the University’s long-standing commitment to the admission and training of California students pursuing future careers in the health professions.
University of California’s 20 health sciences schools are:
|
|
- Pharmacy (UCI, UCSD, UCSF)
|
- Medicine (UCD, UCI, UCLA, UCR, UCSD, UCSF)
|
- Public Health (UCB, UCLA, UCSD)
|
- Nursing (UCD, UCI, UCLA, UCSF)
|
- Veterinary Medicine (UCD)
|
|
|
|
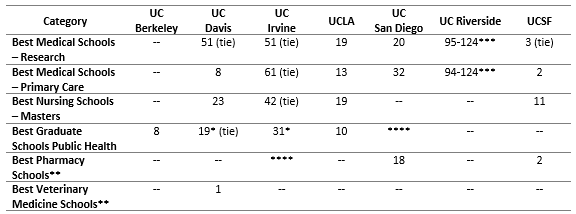
The caliber of UC’s health professional programs is demonstrated in the rankings produced by U.S. News & World Report, current as of April 2022.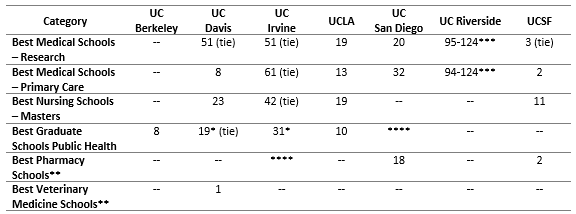
* Indicates a degree program rather than a school.
** Indicates these graduate schools were ranked in previous years and remain current as of publication date. USN&WR does not rank dental or optometry programs.
*** Indicates a grouped ranking.|
****Schools not evaluated. UC San Diego Herbert Wertheim School of Public Health and Human Longevity Science began enrolling students in fall 2020. UCI School of Pharmacy & Pharmaceutical Sciences began enrolling students in fall 2021.
US News & World Report includes a diversity ranking for medical schools. Four of the six UC medical schools are among the top fifteen in the nation for diversity in the rankings published in April 2022.
National Rankings of Medical Schools Based on Diversity
- #3 UC Davis School of Medicine
- #11 UC Riverside School of Medicine (tie)
- #11 UCSF School of Medicine (tie)
- #14 David Geffen School of Medicine at UCLA
To make progress toward health equity, we must have health care providers who reflect the diversity of our communities. Health sciences graduates must be prepared and better trained to address the cultural, social, and economic factors, health practices, and potential environmental hazards that affect health outcomes. In 2004, UC launched a systemwide medical education program intended to help address state needs, collectively referred to as “UC Programs in Medical Education,” or UC PRIME. These medical student educational programs include innovative training opportunities focused on meeting the health needs of California’s historically underserved populations. In the 2021–22 academic year, 366 medical students (more than ten percent of all UC medical students) were enrolled in the six UC PRIME programs. New funding from the State will enable growth in PRIME enrollment over six years, including the launch of new PRIME programs focused on American Indian/Alaska Native communities and those facing Black/African American groups and communities.
Additional efforts toward diversifying the physician workforce and training them to effectively serve communities impacted by health disparities are occurring at UC teaching programs in the central region of the State. UCSF Fresno is the largest physician training program between Sacramento and Los Angeles, with 600+ physicians and rotating medical students trained each year and 550,000+ patient visits annually at clinical partner sites. Approximately 40 percent of all UCSF Fresno 2021 physician-trained graduates remain in the Central Valley.
At UCR, the School of Medicine has recruited nine classes of high-quality, diverse students. The current first-year class is composed of 86 matriculants: 63 percent are female, 41 percent self-identify as being underrepresented in medicine. In addition, 56 percent of students in the current first-year class are from socioeconomically and/or educationally disadvantaged backgrounds, approximately 63 percent have ties to the region, and 35 percent are the first in their family to complete a bachelor’s degree.
Following four years of medical school, graduates enter another period of training — Graduate Medical Education (GME). In March 2022, UC medical school graduates had a ‘match rate’ of 99 percent into GME residency programs and of those, 41 percent matched at a UC hospital. GME programs provide in-depth training that may last three to seven years depending on the area of specialization. All of UC’s academic health centers provide GME training programs and fund a substantial number of them without traditional federal support. In the 1960s, Medicare began paying for a substantial portion of the cost of residency programs. In 1997, it limited the number of funded residencies. The cap on Medicare-funded residencies has not been revised upward since then, despite a growing and aging national population with more health care needs. As a result, and in support of its teaching and public service missions, UC academic health centers began absorbing costs for residency training positions. In the 2020–21 academic year, UC trained 5,266 medical residents. Of those, 860 positions receive no direct federal GME direct support, resulting in an annual cost of $113 million to the University.
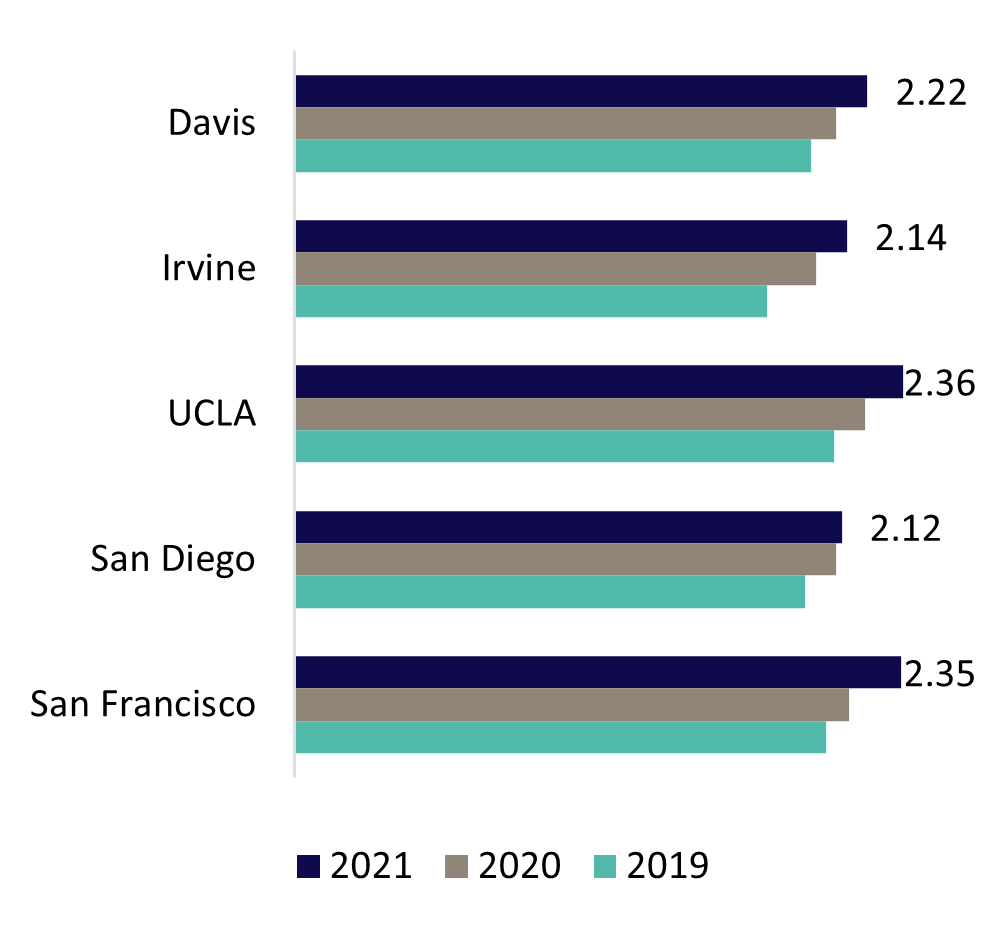
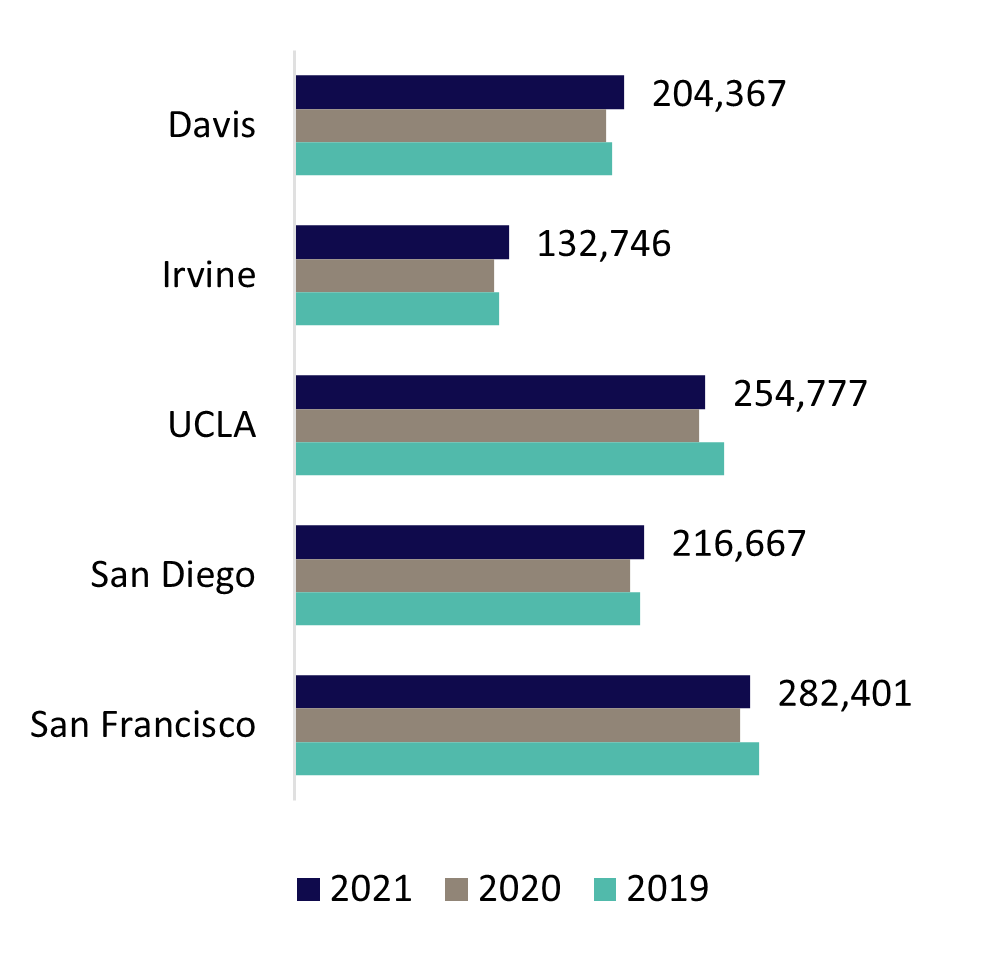
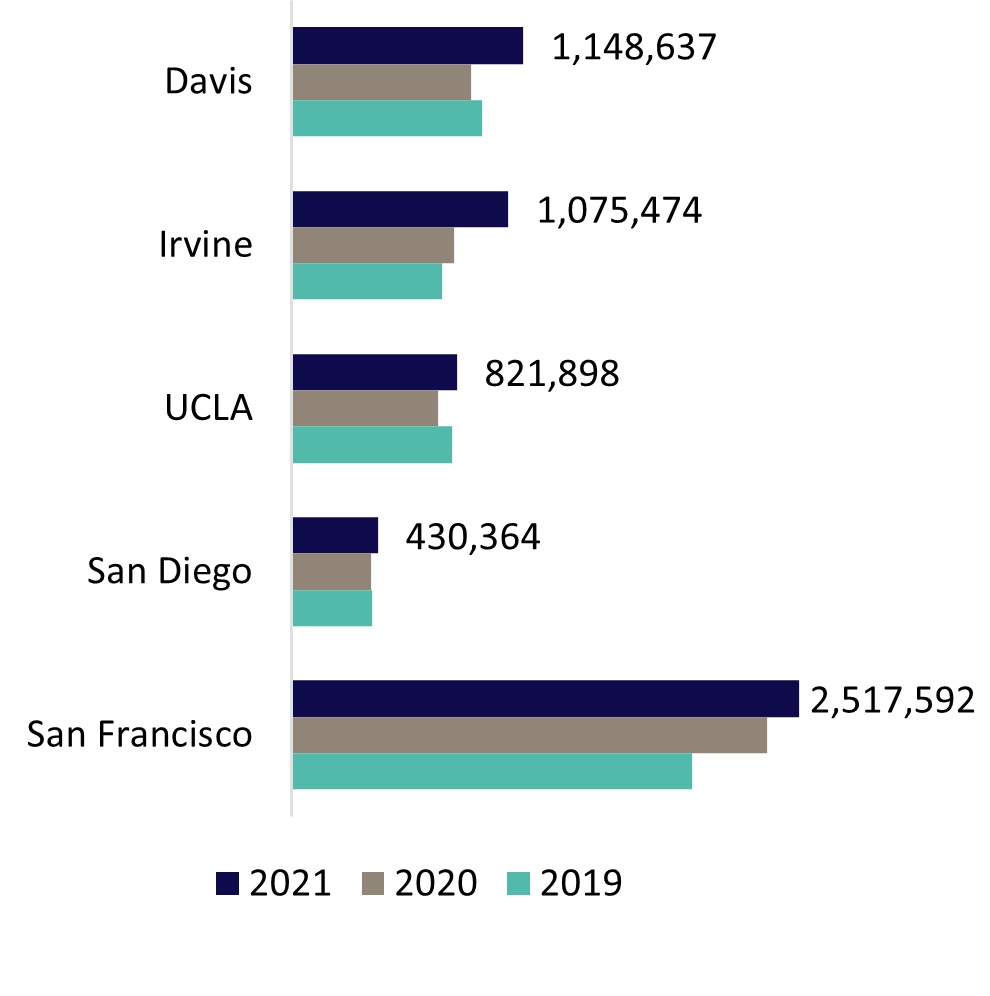
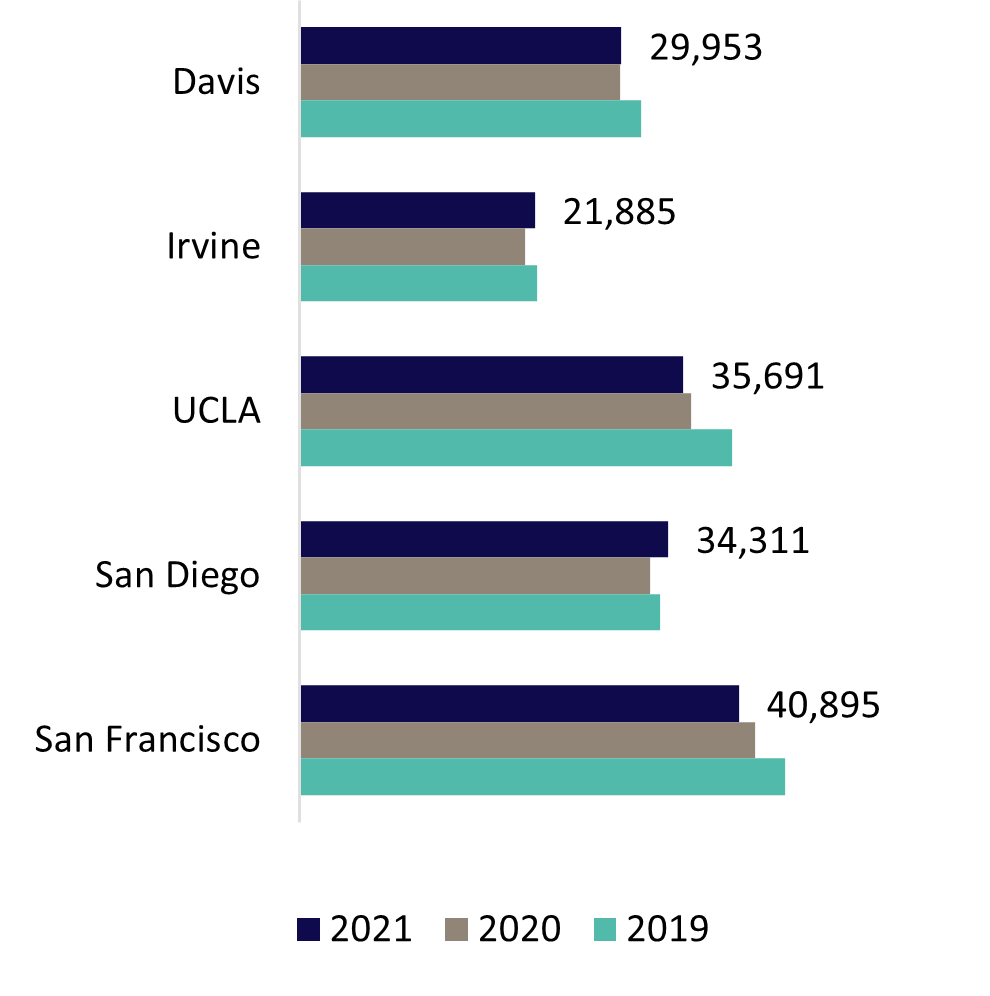
delivering quality, accessible care
UC’s health system includes six academic health centers, five of which own or operate their own hospitals and one that leverages a community-based training and care delivery platform. The hospitals of UC Davis Health, UCI Health, UCLA Health, UC San Diego Health, and UCSF Health admitted 162,735 patients in FY 2021 for 1,090,958 inpatient days. The hospitals also provided 5,993,965 hospital-based outpatient clinic visits. When combined with outpatient services of the health professional schools, University of California Health provided nearly 9.3 million outpatient visits. The care delivered is often for patients with complex medical conditions as shown by the system’s 2.25 Case Mix Index weighted average, which was higher than the levels reported by 96 percent of other California hospitals in FY 2020, the most recent year statewide data is available.[1]
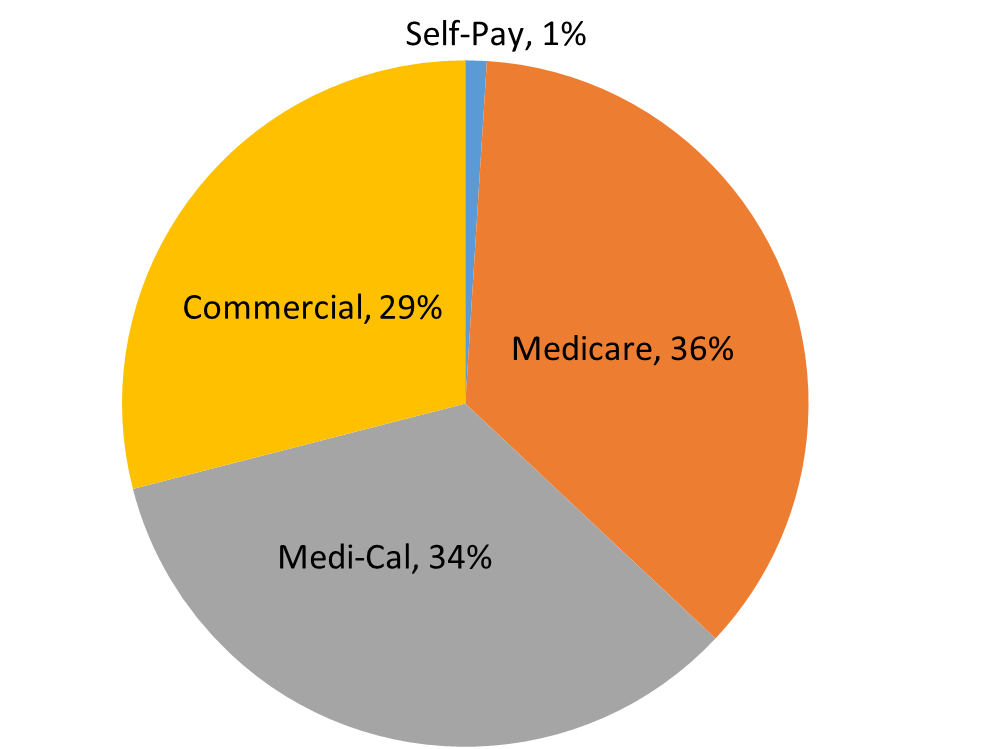
UC’s health system is an essential part of California’s health care safety net system. Care is provided regardless of whether a person has health insurance or the type of health insurance they have. The academic health centers are supported almost entirely by reimbursement for clinical services paid by Medi-Cal (Medicaid), Medicare, and commercial payers. Systemwide, in FY 2021, 34 percent of inpatient days were associated with Medi-Cal, 36 percent with Medicare, 29 percent with private market payers, and one percent with self-paying patients. Together, UC’s academic health centers are the second-largest provider of Medi-Cal hospital services by most measures, despite operating less than 6 percent of the acute care beds in the state.[2] Additionally, UC providers help ensure Medi-Cal enrollees have reliable access to primary care by providing services at Federally Qualified Health Centers. In FY 2021, UC also provided $2.6 billion in unreimbursed care including care in excess of reimbursement for patients with health insurance from publicly sponsored programs such as Medi-Cal and Medicare.
Clinical quality is an area of distinction. All five UC academic health centers that own or operate hospitals are ranked among California’s top hospitals, and two are on the national honor roll, according to U.S. News & World Report, which has ranked hospitals for more than three decades.
[1] Case Mix Index for California hospitals from California Health & Human Services Open Data Portal data.chhs.ca.gov/dataset/case-mix-index/resource/3ed58730-7dbb-4a48-bae5-0e66929c44f7?view_id=506617c4-8b11-4a21-bff6-b2eb7298c9cb
[2] American Hospital Directory cites 74,925 non-federal, short-term, acute care staffed hospital beds in CA. ahd.com/states/hospital_CA.html
The 2021–2022 Best Hospital rankings for UC hospitals are:
| Best Hospitals, Nationally |
Best Hospitals, California |
| #3 UCLA Health |
#1 UCLA Health |
| #9 UCSF Health |
#3 UCSF Health |
|
#5 UC San Diego |
|
#7 UC Davis |
|
#15 UCI |
UC’s health system is known for giving patients access to medical research discoveries and innovations through clinical trials. The approximately 4,700 clinical trials happening across the UC system involve new vaccines and drugs, new technologies for diagnosing and treating illnesses, and new strategies for staying healthy – and include work in areas ranging from cancer and diabetes to COVID-19 and transplants.
Health care for UC students is also a priority. UC’s ten Student Health and Counseling centers offer a wide range or primary care medical and mental health services to UC’s student populations, including primary care, ancillary services such as lab and x-ray, pharmacy, counseling, and psychiatry as well as specialty care, available at some campuses. Additionally, Student Health and Counseling centers have collaborated with UC’s academic health centers to build the capacity to make available a comprehensive array of reproductive and sexual health services to all students who desire them, including health education, screening, prevention, prophylaxis, and treatment for sexually transmitted infections including HIV, and extensive birth control methods including long-acting reversible contraceptives and medication abortion. Students are provided easy, affordable access to care through UC’s self-funded Student Health Insurance Plan (UC SHIP) that offers high-quality, low-cost health insurance to all registered students, with medical, prescription, dental, and vision benefits. The plan is one of the largest self-funded student insurance plans in the United States, with current enrollment of approximately 130,000 students.
delivering more together
The work to improve health equity is an area of priority for collaboration. The Quality & Population Health program brings expertise and resources together from across the system to improve care and outcomes, including for individuals who face challenging social and economic situations. The foundation for this work is in the increasingly complex use of data to identify and understand health disparities, which has been enhanced through new dashboards developed with the Center for Data-driven Insights and Innovation. The Quality & Population Health team uses data for more than 835,000 UC ambulatory patients with cancer, diabetes, and hypertension, and those receiving primary care, to measure improvements across the UC systemwide quality metrics it has developed. Quality & Population Health is able to share best practices across the system and has already helped drive an 11 percent improvement across three diabetes and hypertension metrics.
Other systemwide initiatives to address health disparities using data include a commitment to the nationwide Health Equity Pledge alongside approximately 40 other health care organizations. Pledge participants collect, stratify, and review data about race, ethnicity, language, and sex across top metrics and will share anonymized, aggregate-level information to inform best practices across the country. Additionally, CORDS — a unified, secure data set created at the system level during the COVID-19 pandemic — now has more than 640 million data points. The CORDS data set is a robust resource for UC researchers investigating COVID-19, resulting in 15 peer-reviewed papers and numerous research abstracts to date as well as state and national media attention.
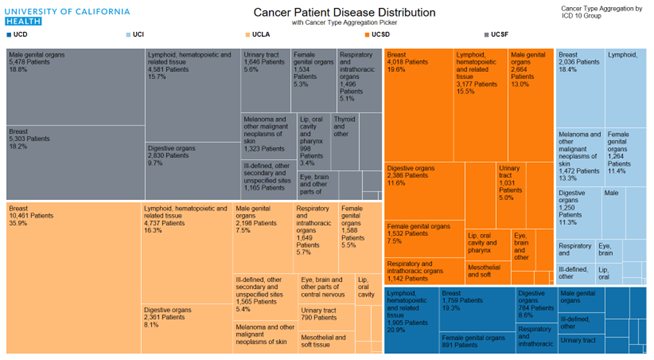
Cancer is another area in which UC’s combined health expertise adds value for patients. The UC Cancer Consortium brings together the University’s five comprehensive cancer centers, each of which holds the highest designation from the National Cancer Institute. Together, these centers collaborate on research and clinical trials, share best practices to provide the highest quality care, and promote health equity by addressing cancer health disparities, including for 10,000 active cancer patients covered by Medi-Cal who received care last year through one of UC’s cancer centers. A new initiative has been the pilot of a multi-campus molecular tumor board where physicians and researchers come together in a collaborative forum to discuss new cancer therapeutic options based on each patient’s unique biomarker profile.
For more information
University of California systemwide economic, fiscal, and social impact analysis report: UC Health impact (pdf)
UC Budget for Current Operations, 2022-23 (pdf)
UC-trained health professionals in California (dashboard)
Medical Centers Annual Financial Report (pdf)
University of California Health (website)
More UCH reports and resources (website)